We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Let Data Be Your Guide: Use SDoH Data To Evaluate Program Efficacy
A 2023 white paper published by the American Health Information Management Association (AHIMA) revealed that 8 in 10 healthcare organizations currently collect social determinants of health (SDoH) data. However, they are challenged to collect, code, and use it to support their social programs effectively.
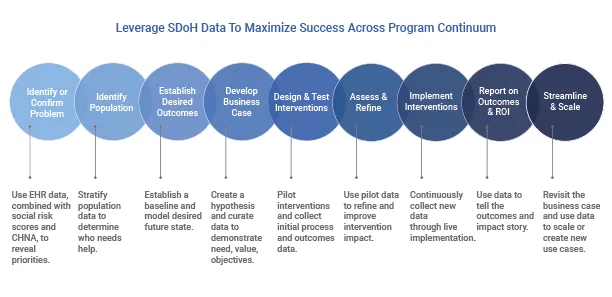
Accessing and using the most appropriate SDoH data is fundamental to identifying and addressing health inequities. From initial program design to assessing return on investment (ROI) and health outcomes, SDoH data plays a critical role throughout the SDoH Program Continuum, as shown in Figure 1. The diagram highlights the steps in the SDoH programmatic journey alongside the potential value that SDoH data contributes to each phase.
The role of SDoH data
Creating a positive impact on health equity and the well-being of individuals and communities can be achieved when the program team and community partners can access, analyze, and use SDoH data effectively.
As SDoH and health equity leaders look to launch new programs, evaluate their existing programs, or enhance struggling programs, it may be helpful to refer to the continuum in Figure 1 and the guidance below to glean a fresh perspective and approach leading toward better health outcomes.
Evaluating ROI requires a clear business case
While each step in the continuum is important, step 4 is crucial. Achieving desired outcomes and ROI from SDoH efforts depends on building a thorough and robust business case. Clarity in the problem to address program objectives and whom the program serves establishes current and future states where data can be collected and compared. Measuring the right types of outcomes and having a practical data assessment and reporting process will ensure results or ROI reporting align with the program's initial design.
But which types of measures should a program focus on from the beginning?
Focus on the most appropriate outcomes and measures
Four types of outcome measures enable SDoH and health equity leaders to assess impact over time as well as evaluate the program's operations and processes. These measures include:
- Process and operational outcomes: Reflect the program's efficiency and effectiveness
- Short-term social need outcomes: Shows how well the program met the immediate need
- Intermediate outcomes and health impact: Focus on changes to health and well-being
- Long-term outcomes and impact on healthcare cost and utilization: Quantifies the more significant effect on population health, community well-being, and cost savings.
Many SDoH initiatives try to address a multitude of problems or achieve too many desired outcomes at a time. Focusing on key downstream or upstream aspects of SDoH provides the most significant opportunity for success, particularly during the pilot stage. After proving the business case hypothesis and demonstrating the effectiveness of chosen interventions, teams can then more widely deploy the program and evaluate results. Only when the more extensive initiative shows positive outcomes aligned with initial objectives can the program consider the data to scale further or attempt to address additional or related SDoH issues.
But which specific measures should a program choose for ongoing evaluation?
Choose key performance metrics for ongoing assessment
Measures are built upon accurate SDoH data consistently collected. Performance metrics, chosen in step 3, demonstrate progress toward program goals, yet also echo the issues the program addresses. Once the program decides the types of metrics to track, leaders should select the specific data points that best reflect the desired impact.
For example, measuring short-term social need outcomes may include identifying a transportation resource and providing a referral electronically. The program can close the loop via confirmation with the transportation company or app. Metrics may consist of the number of fully executed transportation referrals and the number of canceled or no-show appointments.
Measuring intermediate outcomes and health impacts could include providing nutrition education, testing that knowledge, and correlating that increased knowledge to better food choices. Tracking behavior change, health-related quality of life, condition-specific outcomes as well as health and functional status are examples of data points that could connect progress from the current state to the future state.
Intervention impacts can take time to pay off
Keep in mind that an intervention's impact may take time to become evident. This situation is where proxy measures and leading indicators can be used during the pilot or initial launch to improve areas or build on successes.
Long-term outcomes that highlight population impact, changes to health, or cost savings could encompass data points like decreased ED visits, less of a particular type of claim or ICD-10 code, decreased charity care costs, or increased shared savings from value-based contracts, as examples.
Lastly, process and operational measures may target efficiencies like time-to-referral, meeting a specific quality standard like HEDIS, or measuring participants before/after engagement and experience.
But how far along the SDoH stream of causation should the program focus?
Design program strategy and interventions based on the stream of causation
Figure 2 represents the stream of causation which health equity scholars use to illustrate how social factors and interventions impact health. Downstream elements include those that healthcare and public health focus on, including morbidity and mortality, access, risk factors, and living conditions. Upstream factors include policies, governance, culture, and community conditions.
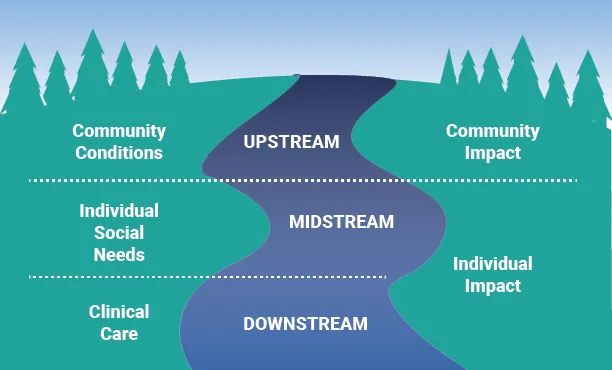
Figure 2: Upstream and downstream SDoH impacts
When designing an SDoH program or intervention, leaders must proactively decide where the effort will focus along the causal continuum or stream. Is a program focusing on individual, community, or societal impacts?
Some initiatives may begin with individual impact and, ultimately, want to change the culture in their healthcare organization to ensure more equitable healthcare. The further upstream an effect can have, the greater potential to positively affect more people within the community.
But what level of intervention is going to support your objectives?
Test what level of intervention is most effective
Analysis of SDoH data provides the iterative input that tells a program team which interventions are working or may need reevaluation. Choosing the most effectual level of intervention is key to ensuring that the program meets its objectives. It is common for teams to select just a couple of interventions without considering or testing the required number of supports that create an impact. Figure 3 shows how the level of intervention becomes deeper as additional or more advanced support mechanisms complement other activities.
Each level of intervention builds from providing information about or referral to a social or community organization to more active coordination, care management, and coaching.
Increasingly, some payer and provider organizations are directly investing in SDoH support. Research published in 2022 found that 78 new SDoH programs, including 57 health systems and 917 hospitals, had made direct financial investments from 2017-2019. These resources were offered directly through the provider organization or a partnership rather than through referral. Most investments went to housing, employment, education, food security, transportation, and social community needs.
Maximizing impact by leveraging SDoH data throughout the journey
The power and value of SDoH data are revealed when specific measures and data points align with clear programmatic or population objectives and support a continuous and iterative quality improvement approach. As the continuum shows in Figure 1, data that helps zero in on issues and priorities are the same data that will reveal the baseline in the current state and represent progress on the business case toward achieving the future state.
RTI Health Advance supports SDoH data across the continuum
Health equity journeys begin or begin again by collecting, curating, and assessing the best data available. Our team has the experience and expertise to ensure the right data is on deck—including our proprietary social risk scoring tool—but also to guide SDoH initiatives toward aligning needs with intervention and quality improvement processes. Contact us to learn more.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.