We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Where Is Quality Measurement Going? Exploring The CMS Universal Foundation
A recent New England Journal of Medicine article acknowledges that a lack of alignment across CMS quality programs confuses and challenges clinicians and health plans. The organization has set forth 20-plus quality programs in its 20-year history of creating transparent quality performance information, driving better accountability in the interest of improving US healthcare. Yet the lack of alignment creates a “tension between measuring all important aspects of quality and reducing measure proliferation."
To address the misalignment, CMS has proposed a building block approach called Universal Foundation. The new model focuses on quality measures that will create “more parsimonious sets of measures" to focus provider attention and drive quality improvement and care transformation. The foundation will apply to many CMS quality rating and value-based care programs.
CMS seeks to address quality measurement burden and confusion
The proliferation of quality measures has created some untoward effects, including:
- Health plan and provider leaders and clinicians are overwhelmed with performance reporting
- Quality measures are misaligned for common clinical scenarios
- Health plans have created their own quality measures
- Lack of clarity when providers and payers prioritize meaningful outcomes that align with national goals
- Multiple processes for measure selection and approval have made implementing aligned measures challenging
- Inconsistent value-based care incentives and rewards
This lack of cohesiveness and added administrative complexity create further disjointedness among payers, leaving provider organizations unsure of which quality measures to work toward.
Quality measure alignment is vital to streamlining focus and elevating national priorities. The Universal Foundation supports this by identifying CMS's priority areas for measurement and revealing gaps.
CMS Universal Foundation goals
As the CMS implements its National Quality Strategy, the Universal Foundation component strives to achieve 7 goals:
- Focus measures that are meaningful to the health of broad segments of the US population
- Address provider burden by streamlining and aligning measures
- Advance health equity by supporting measures that reveal and track care disparities within and among diverse populations
- Transition from inefficient manual reporting to automatic digital reporting
- Enable comparisons among various quality and value-based care programs
- Reveal the forces driving quality improvement and those that hinder it
- Move toward using outcome and patient-reported digital measures
Ultimately, the Universal Foundation should follow a person's lifelong care journey, assessing quality from infancy to adulthood, as well as pivotal care events like pregnancy or end-of-life care.
How CMS created the Universal Foundation
CMS selected the preliminary adult and pediatric measures shown in Figure 1 by prioritizing the most promising measures believed to help achieve national health and equity goals. They created a cross-center working group that focused on coordination, development, and implementation of the aligned measures.
The working group selected quality measures that best align with many diseases and conditions that create the highest morbidity and mortality in the US, like diabetes, high blood pressure, and cancer. The group will work to review specialty-related measures and those that may align with just 1 program.
Regarding health equity, CMS included a measurement-category domain that will encourage stratification of outcome data where disparities can be identified among and within populations.
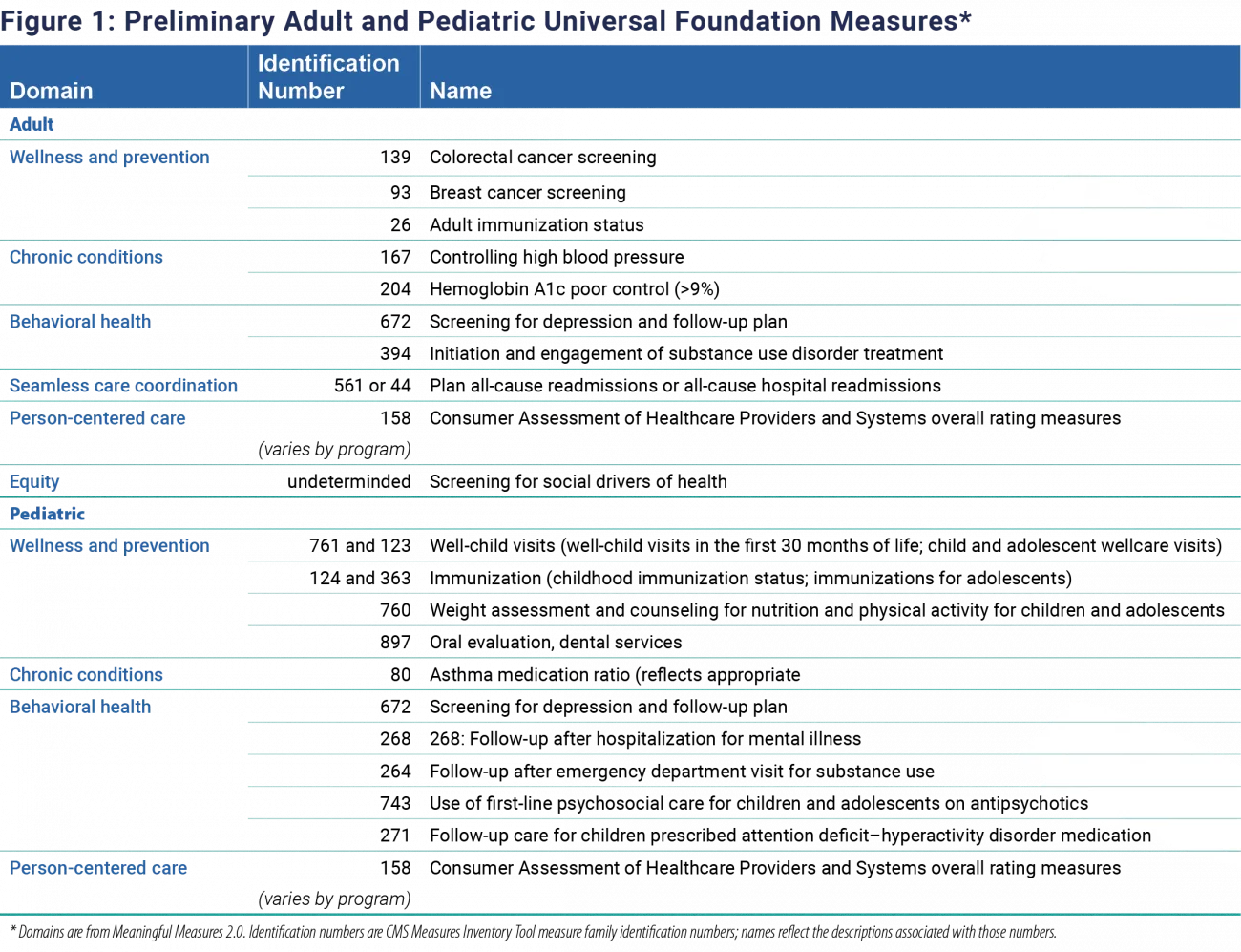
Figure 1: Preliminary Adult and Pediatric Universal Foundation Measures. Source: New England Journal of Medicine
Where does the Universal Foundation go from here?
The CMS working group intends to move forward to align measures while collecting feedback via listening sessions, requests for information, proposed rulemaking, and engagement with the medical community and general public.
The CMS Innovation Center will continue to test new quality measures when appropriate based on the model's quality aims, leveraging the Universal Foundation where possible. With alignment as the primary objective, Universal Foundation measures will be prioritized before other measures that address similar quality aspects.
Outside of CMS, the working group will continue discussing the broader alignment of quality measures. This effort would include the Core Quality Measures Collaborative, the Health Care Payment Learning and Action Network, and states' efforts.
How are healthcare leaders reacting?
Many public social media posts reflect an “it's about time" sentiment. Other leaders demonstrated balanced perspectives.
The American Academy of Family Physicians (AAFP) shared its long-held stance against a “scattershot approach to quality measurement, which requires physicians to report on multiple sets of disparate performance quality measures across a wide array of private and public payers."
AAFP's Vice President of Practice Advancement, Karen Johnson, PhD, expressed that while well-intentioned, CMS's efforts fall short.
“While we appreciate the intent of this announcement, focusing on a smaller number of existing measures that fail to recognize the value of primary care may be a viable interim step but should not deter us from pursuing long-term approaches that better reflect the holistic impact of primary care on outcomes that we care about—better health, smarter spending, and healthier people."
Other leaders, including Jeffrey Susman, MD, the Interim Dean of University of Texas Medical Branch Health's medical school, stressed the need to take this essential first step. He says, “Imagine a day when this plethora of approaches can be reduced to a handful of meaningful measures. CMS has taken an important, imperfect step in that direction." He reinforced that other payers must follow CMS's lead in adopting the Universal Foundation to have a meaningful impact. All payers, including CMS, need to align around measures.
While many will have opinions on what should and shouldn't be included, the intent to develop universal measures is foundational to evolving care quality measurement and improvement.
Representatives from the NCQA applaud the ambitious and much-needed initiative. They expressed their desire to collaborate to reach shared goals to reduce measurement burden, enhance health equity, and transition to digital quality reporting.
Universal Foundation advances quality performance measurement and improvement
CMS has taken the first step to simplify and streamline quality measures in alignment with national health priorities and strategies. Their efforts could deliver a new era of quality improvement with far-reaching effects, including more consistent measures across healthcare organizations and focused performance goals for value-based care.
RTI Health Advance supports improvements in quality improvement strategies and data analysis
Our team of policy, payment reform, healthcare quality, and data science experts collaborate with payers and providers to support changes needed in light of the Universal Foundation. Contact us.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.