We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Depression & The Heart: Understanding Cardiovascular Risk Factors In Women
Heart disease is the leading cause of death in the United States across gender and most racial groups, impacting nearly 700,000 Americans each year. Cardiovascular disease disproportionally affects women and accounts for 35% of deaths annually. This figure exceeds cancer deaths, heart attack, and stroke, yet society still largely associates these conditions as occurring in men. Education is the key to enlighten more women about the risks they may face to their heart health and encourage lifestyle behaviors that may help more women lead longer, healthier lives.
Women experience heart attacks differently
According to a 2021 study published by The Lancet, “cardiovascular disease (CVD) in women remains understudied, under-recognised, under-diagnosed, and under-treated, with women under-represented in clinical trials." The extensive gaps in knowledge regarding women's cardiovascular health can lead to inequities in care. For example, some providers are not well-trained to identify symptoms of heart attack in women. Some women experience no symptoms before a heart attack, while others may report feeling:
- Angina (dull and heavy or sharp chest pain or discomfort)
- Pain in the neck, jaw, or throat
- Pain in the upper abdomen or back
- Nausea
- Vomiting
- Fatigue
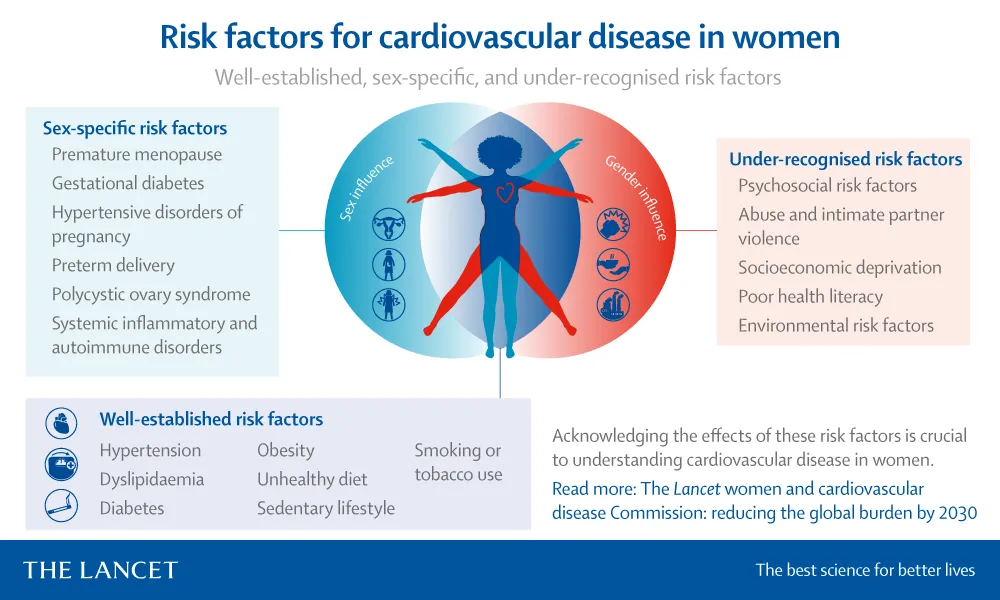
Fig. 1: Known and under-recognized cardiac risk factors in women, featured in the May 2021 "Lancet Women and Cardiovascular Disease Commission" report.
Sex-specific risk factors for CVD in women
The prevalence, presentation, and course of a physical condition can vary greatly by gender. A 2022 study in the AHA Journal asserted that to eliminate gender inequities in cardiovascular cases, providers must adopt a new perspective on cardiovascular health that prioritizes women. “A better understanding of the gaps in knowledge and research needs for CVD in women requires the purposeful adoption of a women-centric approach focused on factors unique to women that affect risk throughout the lifetime," the authors wrote.
There are many physical risk factors for CVD in women, namely:
- Polycystic ovarian syndrome (PCOS)
- Hypertensive disorders of pregnancy
- Gestational diabetes
- Use of oral contraceptives
- Systemic inflammatory and autoimmune disorders (including systemic lupus erythematosus, rheumatoid arthritis, and scleroderma)
- Chemotherapies for cancers more prevalent in women (i.e., breast cancer)
Among the sex-predominant risk factors impacting women are depression and anxiety. The AHA study noted that depression and anxiety “carry an increased risk of CVD, and adverse cardiovascular outcomes in this context are more frequent in women than in men, in particular, at younger ages." According to the Anxiety & Depression Association of America, women are 2 to 3 times more likely than men to experience clinical depression, which is most prevalent between the ages of 25-44. Women also experience anxiety disorders at twice the rate men do.
Depression and heart disease go hand-in-hand
The correlation between heart disease and depression may reflect why women are experiencing cardiovascular disease at younger ages. In the years between 1995 and 2014, heart attacks among the population aged 35-54 grew from 27% to 32%. Among women, that increase was twice as high, growing from 21% to 31% over the same time span.
Depression can impact a patient's energy levels, making it difficult to sustain healthy levels of exercise. Conversely, after a heart attack, women are more likely to develop depression, which increases the risk of developing blood clots, having a repeat heart attack, or suffering a stroke.
“Thirty years of epidemiological data indicate that depression does predict the development of heart disease," says Jesse C. Stewart, Ph.D., an associate professor of psychology in the School of Science at Indiana University-Purdue University Indianapolis (IUPUI).
Adults with a depressive disorder or symptoms have a 64% greater risk of developing coronary artery disease (CAD). Depressed CAD patients are 59% more likely to have a future adverse cardiovascular event.
Societal expectations can place women at risk of heart disease
Many of the studies showing connections between depression and heart disease are observational, making researchers hesitant to use causal language. Nevertheless, depression and heart disease are a significant comorbidity that affects women at all stages of life. Many social factors cause clinical depression in this population group, including:
- Stress related to work and familial responsibilities
- Societal expectations
- Social drivers of health, such as poverty and history of sexual abuse
A survey by the Pew Research Center found that during the COVID-19 pandemic, women were less satisfied with their work-life balance and share of household duties than their male counterparts. This survey showed that the expectation and/or practice of women shouldering most domestic responsibilities had only grown more prevalent during the pandemic.
Societal expectations of women to be “everything to everyone" can contribute to higher levels of stress. The image of the modern woman who does it all requires a type of tug-of-war between multiple roles: career woman, doting wife, devoted mom, responsible daughter, and caring friend. Traditional societal constructs expect women to be all these things while managing the household, supporting school, athletic, or civic interests, and investing in their physical appearance, such as coiffed hair, cosmetics, and stylish apparel. These are complex social roles that each require significant effort and support.
“The societal pressure and expectations that women cope with regularly can increase the chances of developing mental health issues," according to an article by McClean Hospital. "Pressure caused by multiple societal roles and overworking has also been shown to account for poor mental health in women. Women are more likely to be discriminated against as a consequence of their gender when compared to men. This could increase their chances of developing a mental health issue."
“Women are more likely to be discriminated against as a consequence of their gender when compared to men. This could increase their chances of developing a mental health issue."
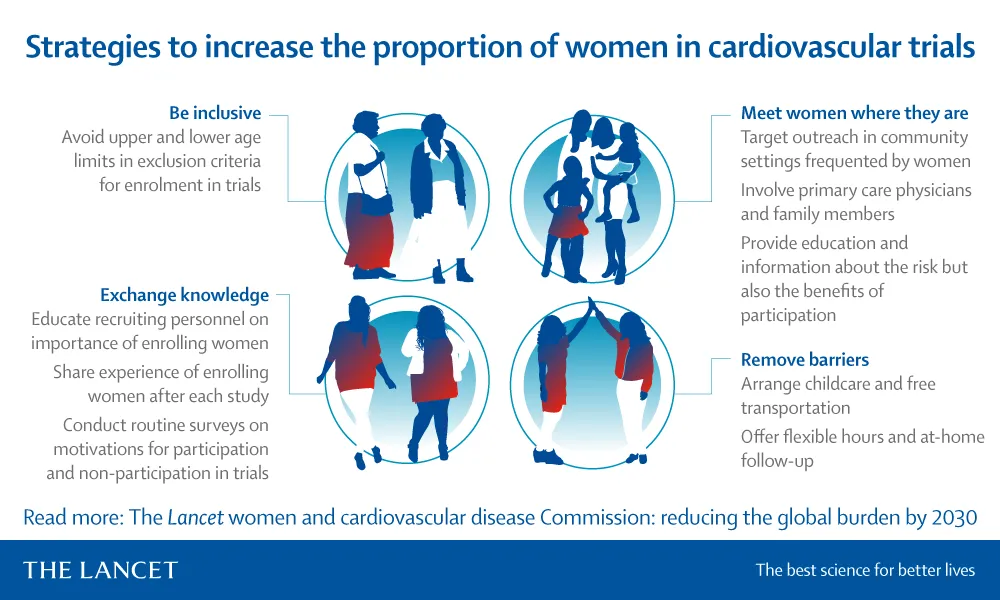
Fig. 2: Strategies to increase the proportion of women in cardiovascular trials, featured in the May 2021 "Lancet Women and Cardiovascular Disease Commission" report.
Emerging discipline targets the biological mind-heart connection
Pyschocardiology, which explores the psychological factors in the diagnosis, treatment, and prevention of coronary heart disease, is a growing discipline expanding our understanding of the relationship between psychosocial distress and the cardiovascular system.
Dr. Lawson Wulsin wrote in the 2012 book, Psychiatry and Heart Disease: The Mind, Brain, and Heart, that “the cardiovascular system and psychological distress are each intimately linked to the central, peripheral, and autonomic nervous systems, the immune system, and limbic-hypothalamic-pituitary-adrenal-gonadotropic axis."
The interconnected nature of the brain and the heart make the management of depression especially pivotal in regard to heart health.
“Unfortunately, some of the symptoms of depression make it challenging for women to take care of themselves and make healthy choices," Dr. Poulina Uddin says. “Often, women with depression sleep too much or not enough, feel fatigued, have little interest in doing things and lack energy–none of which are conducive to sticking with a healthy diet or cardiovascular exercise program."
Identifying early signs of depression
Researchers underscore the importance of managing stress, anxiety, and depression and of knowing your numbers: cholesterol, HDL, LDL, and triglyceride levels; blood pressure; blood sugar (especially for diabetics); and body mass index (BMI).
Treatment options and interventions that center the social and physical dynamics women face are better suited to identify, prevent, and treat cardiovascular disease in women. These options include screening female patients for cardiovascular conditions when they present symptoms that are related to anxiety or depression.
Some of the signs of depression include:
- A change in regular patterns of sleep
- A change in eating patterns, like overeating or not eating at all
- Chronic feeling of hopelessness or dread
- Little interest in activities you typically enjoy
- Difficulty staying focused on daily activities
Beyond this, communities can benefit from astute providers who understand the intricacies of CAD in women and the importance of screening for depression and anxiety to help identify patients who might be at a high risk.
Empowering women's heart health
As researchers and providers learn more about the links between mental health and heart disease, women will be more empowered to initiate lifestyle changes and address potential CAD risks in their lives. Together, patients and providers can build stronger care plans for a healthy heart.
RTI supports cardiovascular health
At RTI Health Advance, we provide the data and experience clients need to increase education, quality, and patient outcomes. Contact us today to learn about our practical population health and health equity solutions.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.