We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Population health management (PHM) has grown in adoption and sophistication as value-based care (VBC) contracts are more prevalent. These events rise concurrently with an increase in chronic diseases, an aging population, and a commitment to the Quadruple Aim. Increasingly, PHM is growing beyond certain diseases to deliver better, more cost-efficient care for various populations at different acuity levels. Maximizing PHM's value – to populations, individuals, and healthcare organizations – requires a more mature data model.
This article is the first in a series of three where we will explore techniques across the PHM continuum, including (1) data capture, (2) analytics, and (3) interventions and reporting.
What's driving population health management adoption?
A 2021 survey of healthcare executives revealed that 98% believed PHM is essential for their organization's future success, and a larger percentage said it was critical. So, what's driving this growth of PHM? Regulatory and financial incentives are top of the list:
- Address cost for highest-acuity patients: Five percent of Americans account for nearly 50% of all health spending with an average of $61K annually, and the top one percent average over $130K in annual healthcare spend.
- VBC contracting: 56% of payers had executed an outcomes-based contract, a type of value-based contract, as of September 2021. Twelve percent of home care companies receive more than 50% of their revenue from VBC contracts.
- An aging population with more chronic illnesses: By 2025, 20% of the U.S. will be over age 65, and 79 percent of people age 70 and older have at least one of seven potentially disabling chronic conditions.
PHM's goals are evolving and expanding
Population health management works to improve health outcomes, prevent increased disease burden, and avoid unnecessary and costly care for specific patient populations but also individuals. Today, PHM is evolving to not only scale current population foci but also provide more continuous and personalized care for "rising-risk" patients with chronic illnesses. CMS, other federal programs, and non-profits like the National Committee for Quality Assurance (NCQA) have also prioritized health equity, providing incentives and guidelines to make healthcare more equitable across populations.
Data is the lifeblood for sophisticated, scalable PHM
As the PHM discipline becomes more robust with tools, peer-reviewed journals, associations, and research, healthcare organizations can leverage novel technologies, new evidence, and proven best practices, which all require data. Figure 1 represents PHM across each juncture where data is leveraged from inputs and analytics to interventions and reporting.
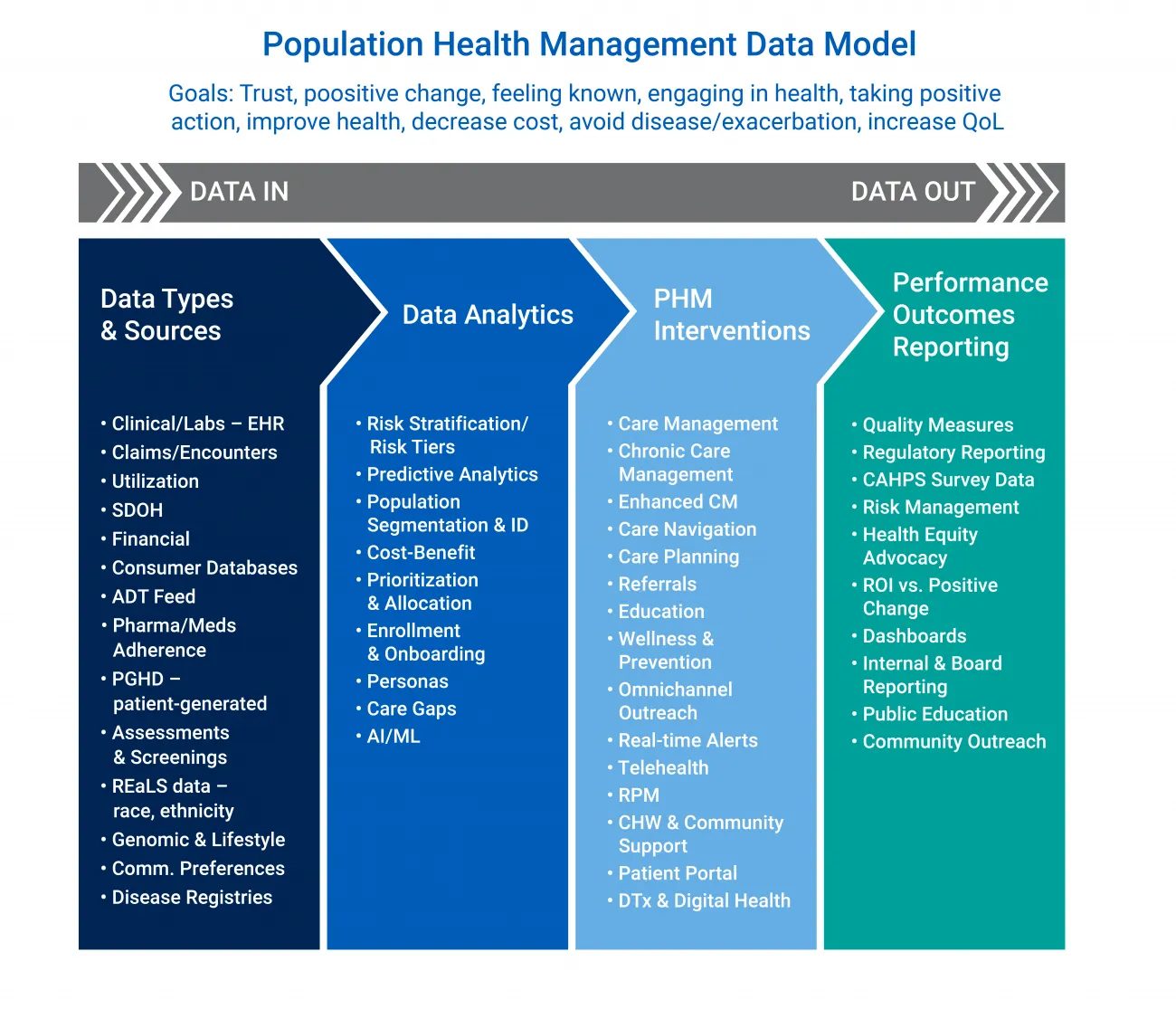
Figure 1: Population Health Management Data Flow Model
A modern PHM program requires a new level of data breadth, depth, and variety. Health systems and payers want relevant, timely, accurate, and aggregated data from a host of sources. In addition to clinical, financial, and encounter information, PHM leaders and managers are including non-clinical, social, and environmental details that play an important role in the success of PHM interventions.
Ensuring that healthcare data is valuable, actionable, and reliable requires a thoughtful architecture that accounts for bidirectional exchanges and implements interoperability tools like HL7, FHIR, and third-party data feeds, as well as health information exchanges and public data sources. Figure 1 lists a variety of data types and sources. Equally important are the connections among these sources.
How mature is your PHM data model?
Maturity level one: Data comes from one or two care settings that may be aggregated across the health system, but it cannot be linked to individual-level data sets.
Maturity level two: Multiple sources deliver high-quality data, some that are real-time, from care or community service locations. Data integration for analytics is possible, and data flows for interventions may use APIs.
Maturity level three: High-value, reliable data flow from many internal and external sources, as well as publicly-available and third-party databases. Real-time and bi-directional exchanges are utilized, and analytics includes predictive modeling and AI/ML capabilities. Patient-generated data may be included. Interventions are driven by analytics, possibly AI, and automated triggers.
Building a more mature PHM data model
These eight techniques offer ways to evolve and mature a PHM program incrementally. They can be used as part of a pilot or discussed during strategy and planning meetings as a way to refresh a PHM program's data flow.
Prioritize data points
There are some standard data types and forms that most PHM programs want to capture and pull into the larger PHM data flow. Program leaders may strive to expand inputs to drive novel analytics, manage new populations, and support broader interventions. For example, "lab values are responsible for 60-70% of all critical clinical decision-making such as admittance, discharge, and medication, according to one highly cited study." Yet, they have been leveraged only in recent years as part of PHM data capture.
- Do you need more information on the patient's physical environment and neighborhood?
- What new data around healthy behaviors would be valuable now?
- Are there gaps among clinical, financial, and consumer data that might be useful to address?
- Do you have a care delivery channel that is not being captured and used but should?
Leverage SDoH data
More than the data-du-jour, socioeconomic data are seen as critical to understanding individuals within a broader context, uncovering unmet needs, and connecting environmental and personal factors to creating positive change in partnership.
Since the Centers for Medicare & Medicaid Services (CMS) provided guidance with the goal of addressing health disparities, socioeconomic data is influencing conversations and PHM decisions. SDoH data is highly valuable because it can inform risk stratification, segmentation, communication, and intervention throughout the healthcare journey.
For example, RTI Rarity™ provides predictive analytics that can project chronic diseases and treatment costs, supporting risk identification by measuring and adjusting for behavioral and social factors that impact health. It's another data source to identify people who are most at-risk for lifestyle-driven chronic diseases.
Paint a multi-source portrait of populations
Publicly-available data sources can provide richness to internal data sources. For example, the CDC/ATSDR Social Vulnerability Index uses 15 U.S. census variables to identify communities that may need support before, during, or after disasters, socioeconomic status, household composition, minority status, or housing type and transportation.
Databases like the Centers for Disease Control & Prevention Datasets, public-use data files and documentation, and healthdata.gov are sources available through the federal government. Most universities that conduct federally-funded research, like the University of California San Francisco (UCSF), Stanford, and Texas Tech, publish collections of databases.
Beyond public sources, many reputable third-party healthcare and consumer data vendors provide de-identified databases or live connections to a data exchange where patient data is de-identified and tokenized. As a data analytics and PHM partner, RTI Health Advance routinely works with client-owned data and contracted third-party data sources of various types.
Interoperability and infrastructure are key
If data is the lifeblood of PHM, interoperability is the veins that are foundational to interconnected, particularly real-time, data sources. A more mature data model can deliver holistic population health analysis by connecting, consolidating, and aggregating disparate but complementary data assets. The height of PHM maturity might be seen in bidirectional data exchanges where value and insights can flow among organizations and, maybe, back into the patient electronic health record (EHR).
Connected data provides the possibility of a comprehensive, longitudinal health record across multiple settings along the patient's journey. Whether through a health information exchange (HIE), individual interfaces, or APIs, CMS' push for interoperability comes from recognizing that the Quadruple Aim cannot be achieved without robust and secure data transparency and sharing.
Improve quality at data gathering gateways
One of the most-heard complaints from patients is about the number of times they have to repeat their information or complete a form. PHM effectiveness hinges on accurate data that demonstrate providers know their patients well. As patient satisfaction receives greater emphasis and weighting, data accuracy and how well it's used will become a moment to build greater patient trust and rapport. Each point of contact is a data gathering gateway, an opportunity to improve data quality.
- What are your data gathering gateways, and how could each contact enhance your data quality?
- In your PHM program, who's responsible for various data pieces?
- And, when are those pieces collected?
- Where are the most mistakes made in data gathering?
- Are those individuals clear on the value of the data they are collecting and how it will be used?
Maximizing two essential tools: screening and assessment
In addition to supporting pre-screening and onboarding to a PHM program, the initial assessment and further screenings gather data paramount to downstream PHM success. These points of contact provide an opportunity to build a positive patient relationship from the onboarding.
An assessment consists of a more comprehensive intake, using a set of questions to determine potential risk factors or barriers to care. They should uncover health goals and priorities, and create treatment recommendations with and possible referrals for specific screenings. A health screening may include a shorter process and set of questions, focusing on a specific risk area, barrier to care, or area of concern.
PHM leaders and managers should ensure that all assessment and screening tools align and support the program's goals and be reviewed for diversity, equity, and inclusion principles to protect against bias.
Data must have value to the patient to build trust
A PHM program may focus so much on getting the right data that patients feel they are no more than the sum of their data points. Creating an open flow of sharing requires that patients understand and experience the benefits of sharing their data. What's in it for them to share their SDoH information? Are the benefits clear? How will sharing lead to improved patient access, resources, or care solutions? How can we build confidence in our data security and privacy measures?
Patients experience high levels of "data fatigue," and every form, conversation, survey, and intake process should be considered within the whole give-and-take in a PHM care relationship. When done well, PHM programs see higher low response rates, more accurate data, and greater trust in the system.
Data that drive personalized, preference-focused communication
As we'll explore in this three-part series, PHM interventions are where data realizes its highest purpose: engaging patients to take positive action. Gathering relevant, timely, and accurate details on a patient's communication preferences helps deliver alerts and trigger action in a way that they desire. Omnichannel outreach can be tailored to have the best impact at the right time. Plus, analytics finds its most significant value when messages are personalized and account for diversity, inclusion, and equity themes.
RTI Health Advance brings together the power of data analytics, digital health, and patient experience to help provider and payer organizations build population health management programs that are mature and aligned with organizational objectives.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.