We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Comparing Major Health Equity Frameworks & Measures
There are two types of quality measures: those that are regulatory-driven – required or incentivized by the Federal government – and measures recommended from healthcare organizations and programs, including federal departments and other non-profits, think tanks and research entities.
As follow up to article one on recent health equity regulations, this article provides an overview of the major health equity frameworks and measures that are forming how health equity performance will be implemented and quantified.
Health equity measures standards
At this time, there are no national standard methods for capturing data on health equity variables. Additionally, there are no standard measures for assessing health equity improvement outcomes. To create accountability and transparency, both are essential.
Research into identifying health equity measures, best practices, and strategies found limited resources. Yet, recent health equity activity and initiatives have ramped up as frameworks, payment models, and accreditation requirements are released from organizations like NCQA, CMS, RWJF and others.
What are health equity measures?
A working definition from the U.S. Office of the Assistant Secretary for Planning and Evaluation and the RAND Corporation, published by the National Committee for Quality Assurance (NCQA) provides a foundation:
“A definition of 'health equity measures' has been proposed to build consistency in discussion and application: an approach to illustrating or summarizing the extent to which the quality of health care provided by an organization contributes to reducing disparities in health and health care at the population level for those patients with greater social risk factor burden by improving the care and health of those patients."
And, because equity and quality measurement are intrinsically connected, it's prudent to look to healthcare quality organizations for accreditation, frameworks, and recommendations health equity measures.
Moving towards health equity performance measures
Even before the Institute of Medicine (IOM) published "Unequal Treatment" in 2003, organizations have conducted research, industry polls, and published recommendations for how to approach health equity data, its collection, analysis, and measurement.
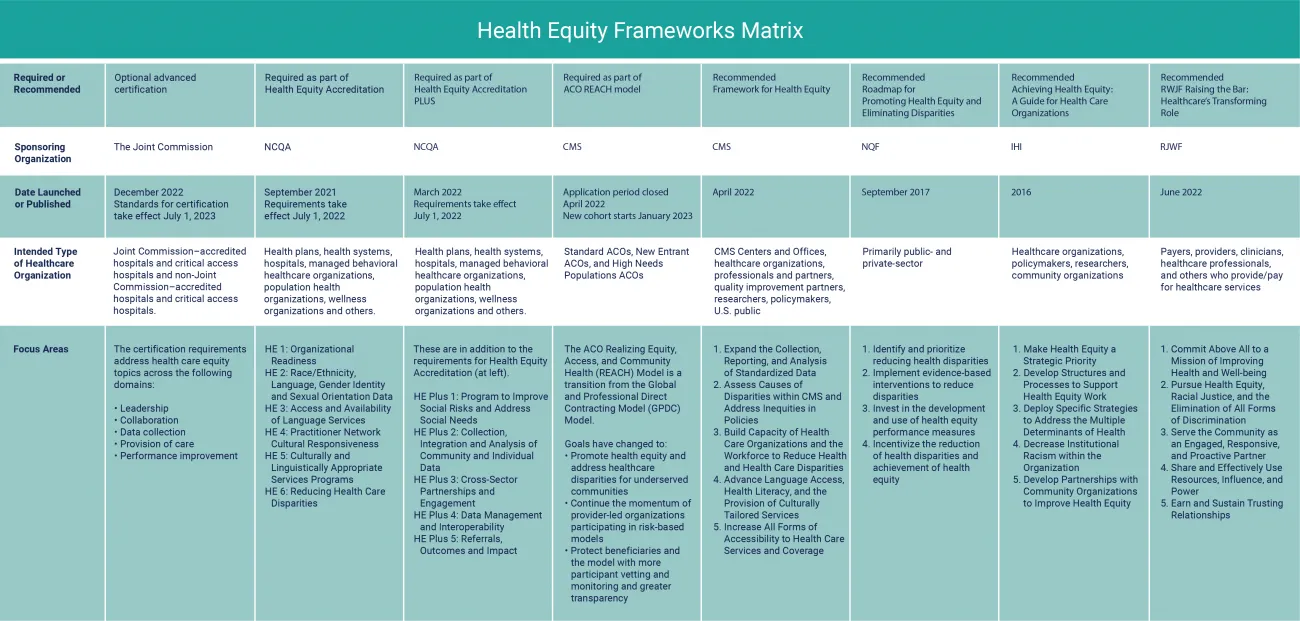
Recent social events and policy shifts are moving health equity measures from ideas to frameworks to requirements. While there are many health equity models and workgroups, we've selected the most prominent health equity frameworks, indicating those with measurement requirements as part of an alternative payment arrangement or accreditation.
Top eight health equity frameworks
See Figure 1 for a health equity framework matrix that covers all of the following. Download a PDF of the matrix here for easy viewing.
The Joint Commission’s Health Care Equity (HCE) Certification
Launching on July 1, 2023, this advanced certification program recognizes hospitals and critical access hospitals that strive for excellence in providing equitable care, treatment, and services. In early 2023, pre-publication requirements were distributed emphasizing the structures and processes that healthcare organizations should have in place to support healthcare equity and reduce health disparities.
The HCE requirements entail healthcare equity topics across 5 domains:
- Leadership
- Collaboration
- Data collection
- Provision of care
- Performance improvement
Health Care Equity (HCE) Certification Resources
News announcement
Health Care Equity Accreditation Standards & Resource Center
Request pre-publication standards (as of 1/17/23)
NCQA Health Equity Accreditation/Plus
Two new accreditation programs replace the Distinction for Multicultural Healthcare that the National Committee for Quality Assurance (NCQA). The NCQA Health Equity Accreditation includes updated standards around health equity and culturally, linguistically appropriate services.
The NCQA Health Equity Accreditation Plus is for organizations whose health equity initiatives are more mature. As of publication, there are 114 healthcare organizations who've received health equity accreditation and seven that have been accredited for the Plus program.
These accreditation designations are for more than health plans. Many organizations are eligible for this accreditation: health plans, health systems, hospitals, managed behavioral healthcare organizations, population health organizations, wellness organizations, and others.
Comparing health equity frameworks: NCQA
The Health Equity Accreditation focuses on:
- Building an internal culture that will influence external engagement
- Culture, linguistic needs and language services
- Identifying opportunities to reduce health inequities
The Health Equity Accreditation Plus goes further, focusing on:
- Community social risk factors and patients' social needs
- Offering social resources
- Partnerships and community-based organizations
- Patient and consumer engagement
- Social need referral processes and partnerships
NCQA Health Equity Accreditation Resources
Distinction for Multicultural Healthcare
Switch to Health Equity Accreditation
Health Equity Accreditation Plus
CMS ACO Realizing Equity, Access, and Community Health (REACH) Model
The Centers for Medicare & Medicaid Services (CMS) redesigned the Global and Professional Direct Contracting Model (GPDC) Model renaming it the ACO Realizing Equity, Access, and Community Health (REACH) Model. Focused on Medicare beneficiaries, ACO REACH is reported to be a temporary model set to expire in 2026 and is expected to serve up to three million patients. As of August 2022, 110 ACOs were provisionally accepted for 2023, which is fewer than half of those who applied.
Comparing health equity frameworks: CMS ACO REACH
This new ACO model focuses on:
- Requiring a health equity plan
- Health equity benchmark adjustment to payments
- Reporting demographic and social needs data
- Enhancing services offered to improve access to care
- Stricter policy on provider-led governance, requiring providers to comprise 75% of the governing board
- Adding beneficiary and consumer advocate representatives to their board
- Compliance with coding practices
ACO REACH Model resource
CMS Framework for Health Equity 2022-2032
As the largest payer in the U.S., the Centers for Medicare and Medicaid Services (CMS) ensures more than 170M individuals through programs like Medicare, Medicaid, Children's Health Insurance Program (CHIP), and the Health Insurance Marketplaces. Their health equity framework was built in alignment with the Healthy People 2000 Framework, which incorporates health equity as a guiding objective for all Department of Health and Human Services programs. In 2015, CMS had published the Equity Plan for Improved Quality in Medicare. That effort is expanded to include more prominence on efforts to increase understanding of disparities, develop and share solutions to reduce disparities, and promote sustainable actions to achieve health equity across the Agency and among their partners.
Comparing health equity frameworks: CMS
The CMS health equity framework focuses on:
- Standardizing data and its widespread use
- Causes of disparities within CMS
- Addressing inequities found in CMS policies
- Increase capacity for organizations and employees to reduce disparities
- Expand access to language and culturally-tailored services
- Improving health literacy
- Greater access to healthcare services and coverage
Because of the widespread influence that CMS has across many health insurance programs, including Medicare and Medicaid, it's actions and requirements have a downstream effect on commercial markets, provider engagements and many other healthcare stakeholders. We'll explore other aspects of health equity through the CMS lens in future articles.
CMS framework resource
CMS Framework for Health Equity
NQF Roadmap for Promoting Health Equity and Eliminating Disparities
With the goal of systematic approach to creating and using health equity measures, the National Quality Forum (NQF), brought together experts to develop a roadmap for how healthcare performance measures and policies could be used to eliminate disparities.
The roadmap recommends four actions:
- Prioritize measures that can help to identify and monitor disparities
- Implement evidence-based interventions to reduce disparities
- Invest in developing and using measures that assess whether interventions reduce disparities
- Provide incentives to reduce disparities
Comparing health equity frameworks: NQF
The NQF roadmap focuses on:
- Uncovering and reducing health disparities
- Evidence-based interventions
- Creating and using health equity measures
- Incentives for performance
In particular, the NQF roadmap describes “disparities-sensitive metrics." These are measures that, among all NQF-validated measures, have a significant disparities quality gap when stratified for race and ethnicity. Figure 2 shows examples of disparities-sensitive metrics.
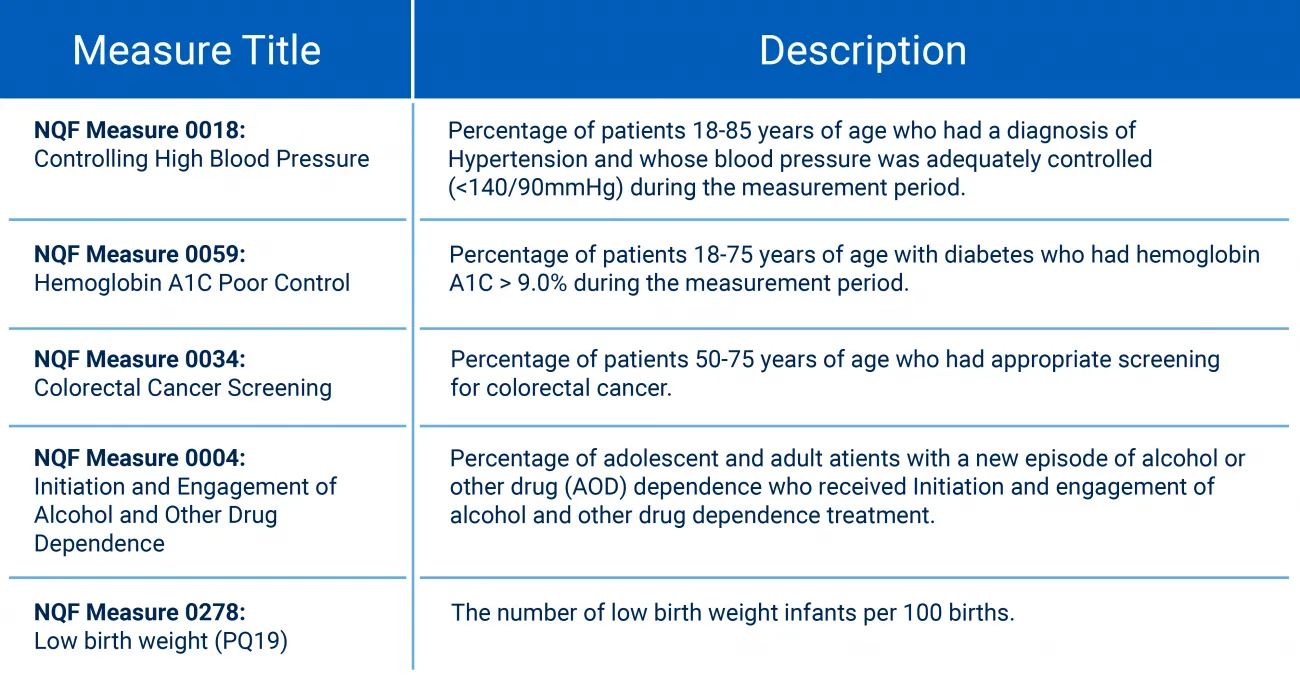
Figure 2: NQF examples of disparities-sensitive measures. Source: NQF A Roadmap for Promoting Health Equity and Eliminating Disparities: The Four I's for Health Equity
NQF framework resources
IHI Achieving Health Equity Guide for Healthcare Organizations
In the Institute for Healthcare Improvement's (IHI) 2021 Pulse Report, they highlight results from a poll completed by 380-US-based healthcare professionals. Fifty-eight percent of respondents said that health equity was a top-three priority in 2021 compared to 25% in 2019. Additionally, 23% said that integrating health equity into outcome measures was the most important thing my organization needs to do to advance health equity.
The IHI's white paper and framework provide “practical advice, executable steps, and a conceptual framework that can guide any health care organization in charting its own journey to improved health equity."
Comparing health equity frameworks: IHI
The IHI framework focuses on:
- Health equity a strategic priority
- Structures and processes
- Strategies to address multiple determinants of health
- Institutional racism within the organization
- Partnerships with community organizations to improve health equity
As part of decreasing institutional racism, the IHI framework suggest assessing the organization's physical space and reducing implicit bias.
How can the physical space help reduce disparities?
- Accessibility by public transportation
- Affordable parking rates
- Easy-to-navigate by signage, walking, wheelchair
How can the organization reduce implicit bias?
- Reviewing policies, structures, and norms
- Training for verbal and nonverbal communication
- Developing strategies like stereotype replacement, perspective taking, and individuation
IHI framework resources
Achieving Health Equity: A Guide for Health Care Organizations
RWJF Raising the Bar: Healthcare's Transforming Role
A broad framework that emphasizes the need for a vision of healthcare's transformation, the Robert Wood Johnson Foundation's work on health equity is built on five foundational principles as shown in Figure 1, including mission, equity, community, power, and trust.
Comparing health equity frameworks: RWJF
The RWJF framework focuses on:
- Four roles and their impact on health equity – provider, employer, partner, and advocate – and three or four key actions each role should take
- Trust and sharing power in relationships and partnerships
RWJF framework resource
RWJF Raising the Bar: Healthcare's Transforming Role
Frameworks viewed through key focus areas
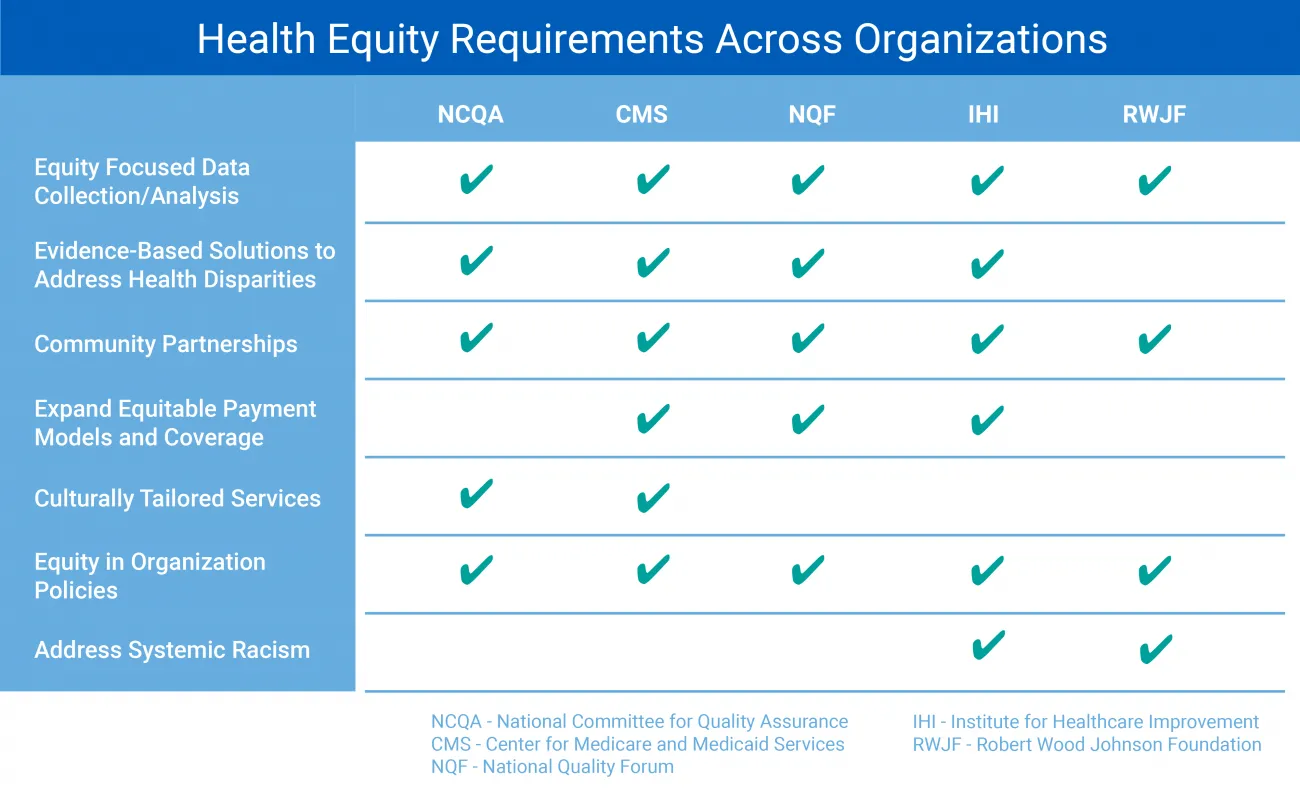
Figure 3: Health Equity Foci Across Frameworks
Which framework will your healthcare organization choose?
Our team supports healthcare organizations in addressing the causes of health inequities. We create practical and effective solutions through data analytics, evidence-based interventions, proprietary artificial intelligence and machine learning platforms, and proven expertise.
Learn more about RTI Health Advance Health Equity Consulting and connect with us today.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.