We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Using The Correlation Between SDoH & Suicide Risk To Improve Prevention
Over the past 20 years, suicide has increased by 30% in the US; it's the 12th leading cause of death for adults over age 25 and second for adults 18 to 25.
Research shows SDoH is associated with a higher risk of suicide
Recent research from the University of Chicago has found correlations between various social determinants of health factors (SDoH) and higher suicide risk. A number of research studies have created lists of specific factors that could be used to identify and stratify the risk of suicide as part of assessment and intervention through existing SDoH programs or as a tailored population health program on its own.
The analysis noted a 56% increase in the suicide rate from the lowest to highest social risk group as well as an 82% increase when comparing the least and most socially vulnerable counties in the US.
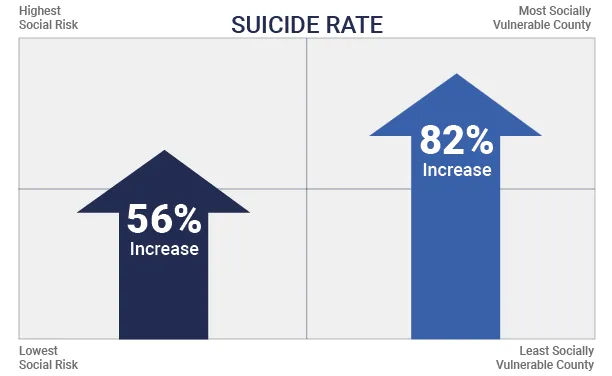
Figure 1: Correlation between suicide rate and social determinants of health
SDoH factors indicating suicide risk
SDoH factors closely associated with higher suicide rates include environmental factors, exposure to violence, access to quality healthcare, and employment status. An individual's age has a pivotal influence on the types of factors that may have a more significant impact on suicide risk. Here, we are focusing solely on adults in the US.
The table below outlines factors in each SDoH category most highly correlated with suicide risk from research studies, which includes the Healthy People 2030 list of 5 social drivers plus food insecurity that was found as an influencing factor.
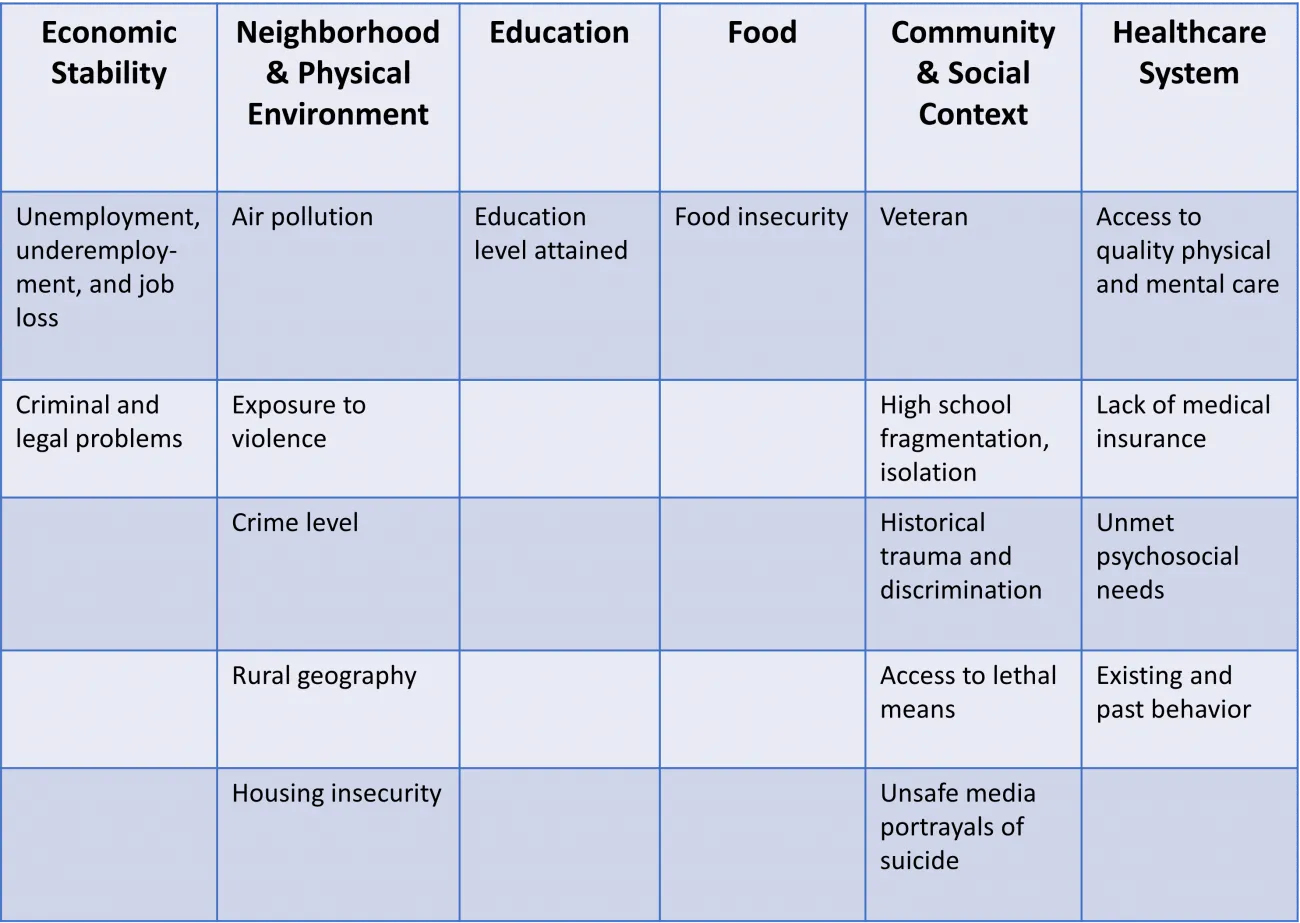
Figure 2: SDoH factors most associated with a higher risk of suicide. Source: JAMA Network
Gender as an additional suicide risk factor
Gender is a well-researched risk factor for suicide. Although women make almost 3 times as many suicide attempts as men, men in the US make up about 80% of suicide deaths. Men use more lethal means of suicide, such as using guns, contributing to their higher death by suicide rates, with the rate rising after a period of decline.
According to the US Centers for Disease Control and Prevention (CDC), age-adjusted male suicide rates in the US increased by around 2% per year from 2006 to 2017, a 26% increase since 1999. CDC research reveals that certain groups of men are at particular risk of suicide, including those:
- Who experienced divorce
- Who served in the military
- Who lived with mental illness
- From an Aboriginal background
- Who are age 75 and older, encompassing those with the highest rates of suicide
Tools to stratify and identify who's at higher suicide risk, in need of intervention
While most of the current cadre of SDoH and social risk assessments do not ask questions directly related to suicide, the majority cover topics or factors closely associated with suicide risk.
Assessments like health-related social needs screening tool from the Centers for Medicare & Medicaid (CMS) or PRAPARE® (Protocol for Responding to and Assessing Patient Assets, Risks, and Experiences) cover many factors associated with higher suicide risk, including:
- Income, employment, and money worries
- Veteran status
- Housing instability and concerns
- Medical insurance coverage
- Education level
- Social connections and isolation
- Personal safety and abuse or violence concerns
- Alcohol and illegal drug use
- Mental health issues like depression, anxiety
- Gender
The challenge that care teams face is that unless asking directly about suicide or conducting a suicide risk assessment, a patient's heightened risk could be overlooked. Data science and technologies like artificial intelligence (AI) and natural language processing (NLP) are bringing greater attention to suicide risk and are proving effective in making the connection between SDoH and risk.
A 2023 published study found that an NLP tool could extract SDoH factors from structured and unstructured electronic health record (EHR) data and associate them with an increased risk of suicide-related death among US veterans.
The NLP-extracted SDOH data included 8 factors:
- Social isolation
- Job or financial insecurity
- Housing instability
- Legal problems
- Violence
- Barriers to care
- Transition of care
- Food insecurity
For these nearly 9,000 men (96.45%) and women (3.55%), the 3 SDoH factors with the most prominent effect were legal problems, violence, and nonspecific psychosocial needs.
Integrating suicidal risk data into SDoH and PHM programs
Social risk indices or AI-NLP tools can be used as an automated scan of structured or unstructured data in an EHR, for example. Or they can be integrated as a data source or feature set into existing population health management or care management tools, enabling alerts when a change in status or new information could indicate higher suicide risk or a need for intervention.
A local area index, like the RTI Rarity™ tool, can be used to supplement existing data for current and new patients or member cohorts to create a social risk score with corresponding suicide indicators that should be explored further in the right circumstance or clinical touchpoint.
Making the connection for suicide prevention
Building off of the proven connection between SDoH and suicide risk, care teams and managers can leverage data from existing tools and assessments in new ways to uncover opportunities to intervene and prevent mental health exacerbation and suicide.
RTI connects population trends to individual needs and risks
RTI supports organizations at the forefront of healthcare. Our team of experts covers the spectrum of issues faced by payers, providers, and vendors today. From health equity and social risk data analytics and programs to quality improvement and population health assessments and program development, we can help you achieve care, quality, and cost goals. Contact us to learn more.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.