We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
As we conclude this three-part series on digital connected care, we discuss what's trending now and what's possible for the future.
Returning to traditional care channels while accelerating connected care use cases
On one hand, healthcare is shifting back to pre-COVID, in-person care. At the same time, digital connected care is accelerating with a host of use cases, research, and pilot projects with visions of the future.
According to the Alliance for Connected Care and analysis of Zocdoc appointment booking data, specialties that were seeing 25-40% of patients virtually in May 2020 were seeing 4-8% virtually in May 2021. The specialties that maintained at least 75-80% virtual appointments were in mental health. Primary care shifted from 58% to 17% virtually.
Yet, published case studies, research articles, and pilot findings show that interest in optimizing virtual and connected care is not abating; it's accelerating. The excitement of possibilities connected healthcare can bring fuels the pace: greater access, more timely care or referrals, faster interventions before escalations, and more care delivered for less cost at home.
As one example, telemedicine visits for outpatient appointments at UCSF Health spiked from 2% of visits in February 2020 to more than 60% by April 2020. When they surveyed their patients, they found that patients were more satisfied with their video visits than in-person. Today, almost one-third of outpatient visits are conducted virtually.
Connected care supports the seismic shift in forecasted healthcare revenue
According to PwC's healthcare dynamic forecasting model, “we're in the middle of a five-year, $1 trillion shift in revenues away from traditional payers and providers." By 2025, they expect that health organizations will have moved into one or more of three new ecosystems. This shift relies on emerging business and care models, as well as connected care technologies.
Vertically integrated models – growing from $180B to $235B – where hospitals, physician groups, and health plans are owned and operated by a single entity.
Virtually integrated models – growing from $840B to $935B – where core capabilities or systems of individual organizations through cost-sharing and risk-sharing agreements, acting as a larger, single entity.
Consumer offerings and analytics – growing from $30B to $300B – where direct-to-consumer services, new care services, and consumer data analytics are created, packed, and sold.
How is connected care research growing and collecting evidence?
Nearly 500,000 articles have been published in peer reviewed journals on some aspect of connected health since the pandemic started. Topics like the following demonstrate that there is real-world evidence that connected healthcare can be an effective, as well as cost- and resource-efficient model of care:
- “Efficacy of telemedicine for the management of cardiovascular disease"
- “Harnessing Digital Health Technologies to Remotely Manage Diabetic Foot Syndrome"
- “Remote Patient Monitoring with Wearable Sensors Following Knee Arthroplasty"
- “Factors influencing the implementation of early discharge hospital at home and admission avoidance hospital at home"
A systematic mapping study, conducted by researchers from seven countries, asked if connected health studies were empirically validated. Their findings, shown in Figure 1, indicated that the majority of the studies were indeed empirically validated, using the following tools:
- 28.3% by case studies
- 26.4% by controlled experiments
- 13.4% with surveys
Non-empirical papers included 12.0% focused on theory and 5.2% using history-based evaluation.
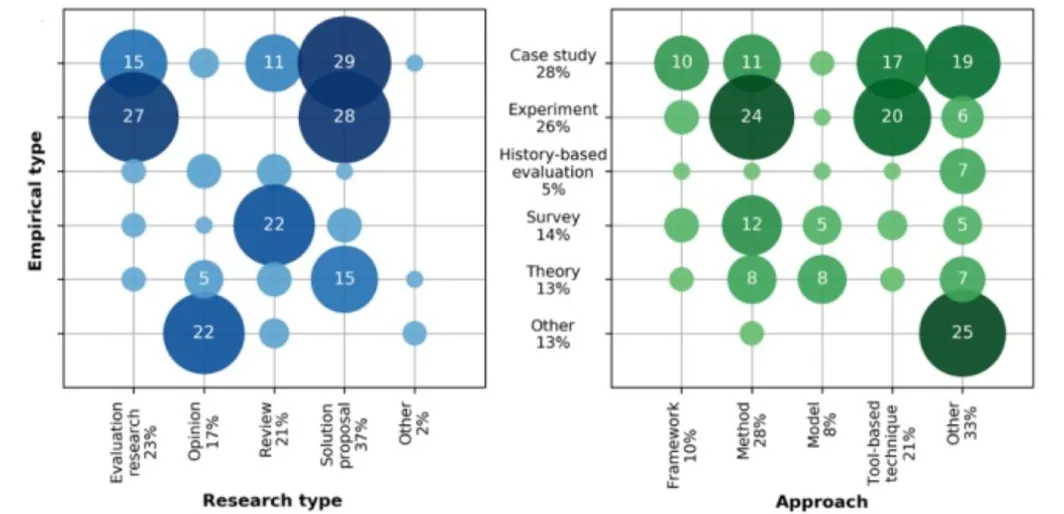
Figure 1: Connected care by empirical and research type and approach.
Copyright ©Maria Karampela, Minna Isomursu, Talya Porat, Christos Maramis, Nicola Mountford, Guido Giunti, Ioanna Chouvarda, Fedor Lehocki. Originally published in the Journal of Medical Internet Research (http://www.jmir.org), 25.09.2019.
Where is connected care gaining traction?
Amongst the various types of technologies and use cases, three that have gained greater adoption during the pandemic and are being adapted for potential long-term use are telehealth (aka virtual care, telemedicine), remote patient monitoring, and hospital-at-home.
The National Telehealth Technology Assessment Resource Center published their 2022 survey that captured what healthcare organizations across the industry are using for connected care technology solutions. Data reflects survey of these organizations in 2014, 2018, and 2022 as shown in Figure 2.
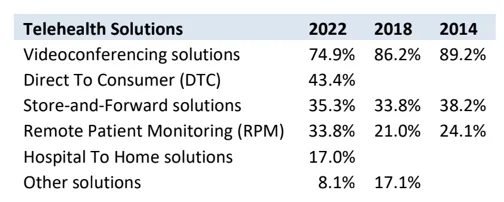
Figure 2: 2022 TTAC National Telehealth Technology Survey
Figure 3 shows what connected care software, services, and systems that survey participants intend to assess, evaluate, or acquire within the next 18 months.
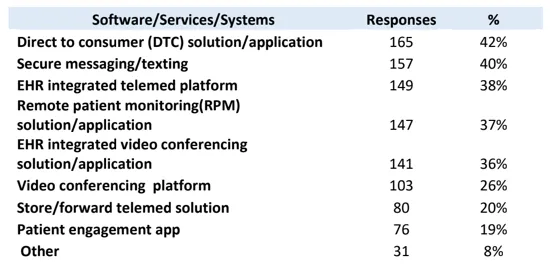
Figure 3: 2022 TTAC National Telehealth Technology Survey
The following connected health technologies may be implemented by 24-25% of survey participants in the next 1-2 years:
- Patient engagement platform
- Artificial intelligence
- Chat bot
- EHR integrations
- Wearable bio sensors
- Robotics
Telehealth
Seventy-two percent of TTAC's 2022 survey participants plan to expand telemedicine in the next one to two years with 22% keeping their level of service the same. And, in February 2022, SimplePractice conducted a survey which found that 88% of U.S. clinicians expected to continue offering a telehealth option permanently. This is aligned to reports of expanding use cases.
Three examples of programs highlight telehealth success:
Veteran's Administration: A five-year grant from 2020 has enabled a research team to expand their telehealth neurology and pain program to provide chronic-pain management via telehealth, and broadening what the institute calls tele-GRACE, extending the reach of geriatric home and community-based care management.
University of Arkansas for Medical Sciences: Research determined that 70% of children received follow-up care through a telehealth referral pathway compared to 30% of in a standard pathway. Children in the telemedicine specialty referral pathway received follow-up care 17.6% faster than those in the standard primary care referral pathway.
Kaiser Permanente: Members in several states can access a 24/7 video health center that connects them to a physician who triages their needs, referring them to the ED when needed. The telehealth service resolves the program 60% of the time.
Remote patient monitoring
A 2022 report published by Walmart Health and Wellness and Medscape released results from a survey of over 10,000 U.S. health care professionals from December 2021 to March 2022. As shown in Figure 4, their research highlighted differences between rural and non-rural clinicians. Of note, 58% of rural clinicians and 55% of non-rural clinicians are comfortable or very comfortable using remote patient monitoring, and 65% of rural clinicians and 70% of non-rural clinicians consider RPM beneficial or very beneficial for patients. This shows potential as 22% of rural clinicians and 28% of non-rural clinicians are currently using RPM.
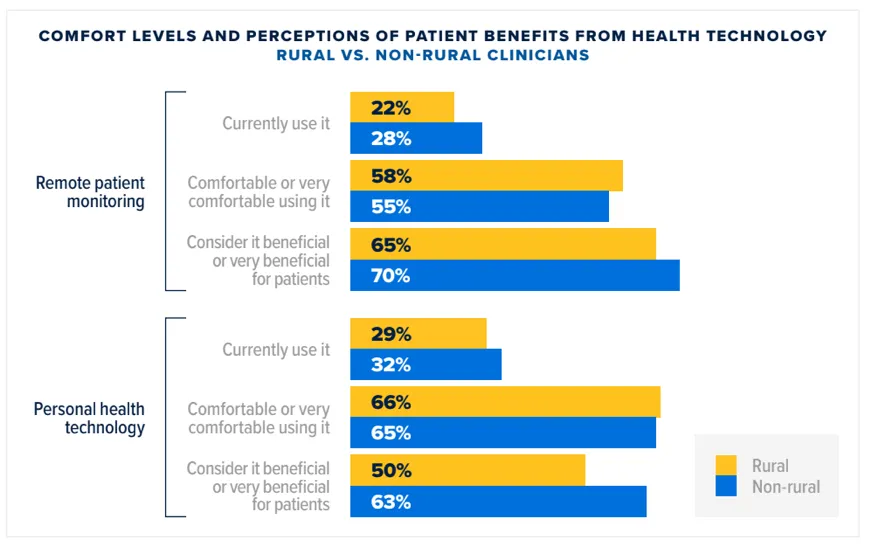
Figure 4: Health Care Professionals' Perspectives on Healthcare in Rural America
Two recent programs highlight RPM success:
Center for Connected Health and Partners Home Care: Over 500 heart failure patients have been monitored remotely, collecting vital signs like heart rate, blood pressure and weight, using simple devices in the patient's home. The information is transmitted daily to a home health nurse who identifies early warning signs, notifies the patient's PCP, and intervenes to avoid a potential health crisis. This program's pilot reduced hospitalizations.
Mayo Clinic: Its RPM program prevented avoidable hospital readmissions and improved patients' recovery from COVID-19. Analysis of data from 7K+ patients in 41 states found that its two-tiered RPM program with nursing support led to positive outcomes, including high patient engagement, low hospitalization, low 30-day mortality.
Hospital-at-home
On the heels of the Acute Hospital Care at Home waiver that began with the COVID-19 public health emergency, high-level care in the home has shown it can be safe, effective, less costly, and deliver greater patient satisfaction.
Kaiser Permanente patients using their hospital-at-home services said their care teams gave higher scores than for traditional inpatient care:
| Satisfaction Score | Hospital At Home | Traditional Inpatient |
| More responsive | 85% | 67% |
| Smoother care transitions | 76% | 52% |
| Overall better experiences | 80% | 71% |
Two recent examples highlight the success of hospital-at-home:
Sanford Health: Sanford is the nation's largest rural health system. Their remote diagnostics program kept 1,000 patients out of the hospital or clinic by providing a comprehensive exam kit to perform a guided, remote medical exam of the ears, lungs, heart, skin, abdomen and temperature. Recently, they announced a $350M gift to create a virtual care center and provide access to care in rural and underserved areas of the Midwest. The program will include a virtual hospital, connecting hundreds of existing clinics, hospitals and long-term care facilities.
JAMA Network Open: A systematic review of nine randomized clinical trial studies, including 959 adult patients with a chronic disease, found that hospital-at-home lowered the risk of readmission by 26%, as well as lowered the risk for long-term care when compared to the inpatient group. “Patients who received hospital-at-home care also had lower depression and anxiety scores than patients receiving in-hospital care, but there was no difference in functional status."
Envisioning the value of connected healthcare
B.J. Moore, the CIO of Providence, a health system that operates 52 hospitals across seven states, sees a high-value and unique importance of connected care. "The future we see is telehealth and remote patient monitoring being at the center of care delivery."
RTI Health Advance works with healthcare organizations to achieve new business models and new models of care via connected healthcare through digital health, care quality, patient experience, population health, data analytics, and health equity services and expertise.
Learn more about RTI Health Advance and connect with us.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.