We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Looking at connected care through an expanded lens
Connected health was a concept in the late 1970s when telemedicine took root to address shortages in care providers. In recent years, however, connected healthcare has grown out of a confluence of population health, value-based care models, digital technologies, interoperability, consumerism, and achieving the Triple Aim. Today, the Quintuple Aim is on the scene, focusing on better outcomes, improved patient experience, lower costs, clinician wellbeing, and health equity. See Figure 1.
Connected healthcare drives the Quintuple Aim
In 2007, the Institute for Healthcare Improvement (IHI) launched the Triple Aim initiative to emphasize the interrelatedness of quality, cost, and experience. It solidified the three most important aims for healthcare regulation, legislation, new value-based care models, and financial rewards. Then, the Triple Aim became the Quadruple Aim in 2014 when research showed that “decreased clinician engagement and burnout directly correlated to lower patient satisfaction, reduced health outcomes, and higher costs." Clinician well-being was added then. Last year, health equity was posited to round out a Quintuple Aim after social injustice came to greater public awareness and the pandemic brought heightened attention to existing health inequities.
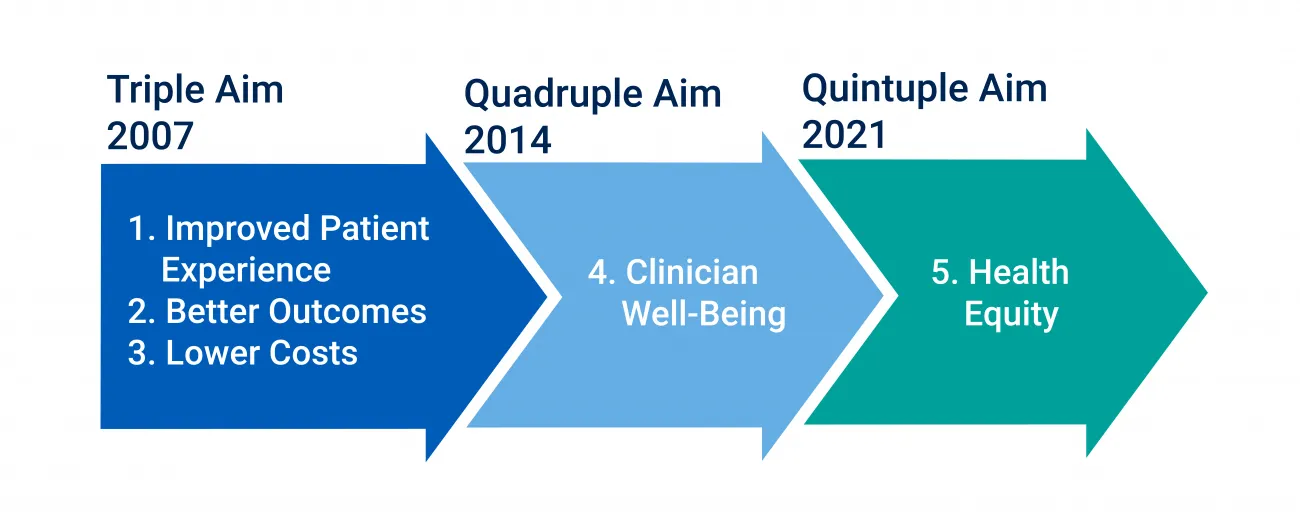
Figure 1: The Evolution of the Triple Aim into the Quintuple Aim.
Connected healthcare is linked to these aims because sharing data, connecting people, and delivering care beyond the hospital or clinic became a strategy aligned to how people work and live. It also provided possible solutions for longstanding issues with access due to health inequities and the diverse needs of rural communities. Connected care holds promise to help clinicians manage burnout and workload and reach historically marginalized populations facing health inequities.
How has the pandemic accelerated connected healthcare?
Any discussion of connected care would be remiss if it didn't highlight the fast-paced shifts that pushed connected care to the fore in response to the COVID-19 public health emergency. Lockdowns and social distancing accelerated the need to scale telemedicine, virtual care delivery, and remote patient monitoring to continue care for existing patients alongside managing as much care outside of the hospital as possible. People who began working from home, including those in healthcare, immediately shifted to using connected technologies.
Three statistics demonstrate the impact of the pandemic on connected healthcare. Telemedicine use increased 63-fold during the early months of the pandemic compared to pre-pandemic, and remote patient monitoring grew 200% from 2018-2020. MGMA surveyed their medical practice members and found that 59% shifted workers to permanent remote or hybrid settings in 2021.
How can healthcare organizations leverage connected healthcare going forward?
As we embark on this series, it's helpful to take a broader view of connected healthcare.
What is “connected" in connected healthcare? And, how are they connected?
While it might seem obvious, it's important to think about the “connected" aspect of connected healthcare. It reveals opportunities and possible solutions when faced with population health, chronic care, team-based care, and value-based care goals or challenges.
The five main pieces that join together in connected care include data and databases, software systems, medical devices, people via communication, and team activity via collaboration. It's all data, however, with the purpose of providing or coordinating care.
The “how" of connected healthcare spans a variety of architectures and technologies. They provide a foundation for data sharing, communication, tracking, and reporting. Regional, state, and national healthcare information exchanges (HIEs) provide various levels of data sharing. There are third-party data exchange services and Cloud solutions that can support additional capabilities like population health data analytics. Lastly, there are many longstanding data exchange standards, including HL7 (Health-Level-7), FHIR (Fast Healthcare Interoperability Resources), CDISC (Clinical Data Interchange Standards Consortium), and others that many healthcare organizations use:
- 95% of healthcare organizations across 30 countries use HL7.
- As of 2021, 24% of healthcare companies were estimated to utilize FHIR APIs at scale.
- 67% of providers and 61% of payers expect their organizations to use APIs at scale by 2023.
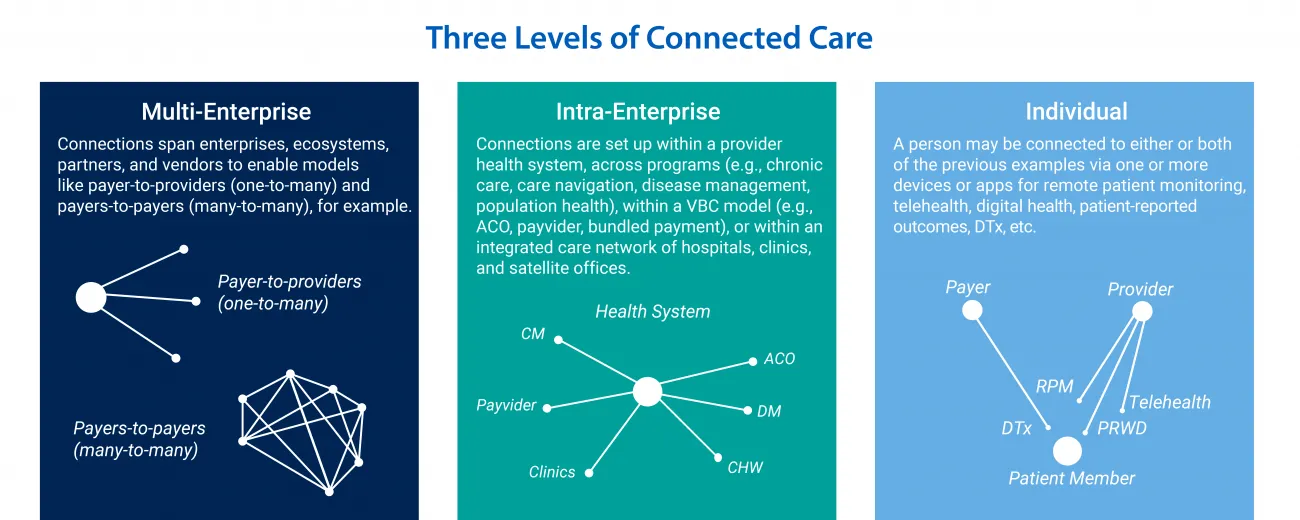
Connected healthcare can be viewed from three levels
This first article in the series sets up the topic, and hopefully conversations, around the value and direction of connected healthcare. To that end, it's helpful to think about any program or initiative that will rely on connected care from three levels:
- Multi-enterprise: Connections span enterprises, ecosystems, partners, and vendors to enable models like payer-to-providers (one-to-many) and payers-to-payers (many-to-many), for example.
- Intra-enterprise: Connections are set up within a provider health system, across programs (e.g., chronic care, care navigation, disease management, population health), within a VBC model (e.g., ACO, payvider, bundled payment), or within an integrated care network of hospitals, clinics, and satellite offices.
- Individual: A person may be connected to either or both of the previous examples via one or more devices or apps for remote patient monitoring, telehealth, digital health, patient-reported outcomes, DTx, etc.
What's next for connected healthcare?
Pivoting from “what is" to where organizations could or should use connected care requires looking into the barriers that slowed down adoption before the pandemic and highlighting what is being done now to overcome those challenges. Article two in the series will focus on those barriers and article three will look at where connected care has had traction – even beyond telemedicine – and considerations for future adoption and use cases.
Driven to deliver evidence-based, practical solutions for business and clinical leaders that advance healthcare for everyone, RTI Health Advance supports connected healthcare and the Quintuple Aim through digital health, care quality, population health, and health equity.
Learn more about RTI Health Advance and connect with us.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.