We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Determining A Health Equity Strategy: Find A Fulcrum
Identifying opportunities for improvement in your health equity strategy
In 2021, 58% of health systems said health equity was a top priority (IHI survey). But, how can payer and provider organizations create momentum, then leverage it to create positive change for patients and the business? One approach is to build health equity strategy “fulcrum points” that can increase opportunities for success.
What is a fulcrum in your health equity strategy?
Think of a fulcrum like the seesaw ride in a child’s playground. But, rather than trying to achieve balance, we want to shift and increase the size of the fulcrum to create more remarkable results from health equity efforts. This is particularly true with tight population health budgets and limited time.
How can healthcare and equity leaders you gain leverage to cause positive change that improves health outcomes? Part one of this two-part article series explores the first three of six “fulcrum points” to create that force for good.
Fulcrum 1: Health equity versus health equality
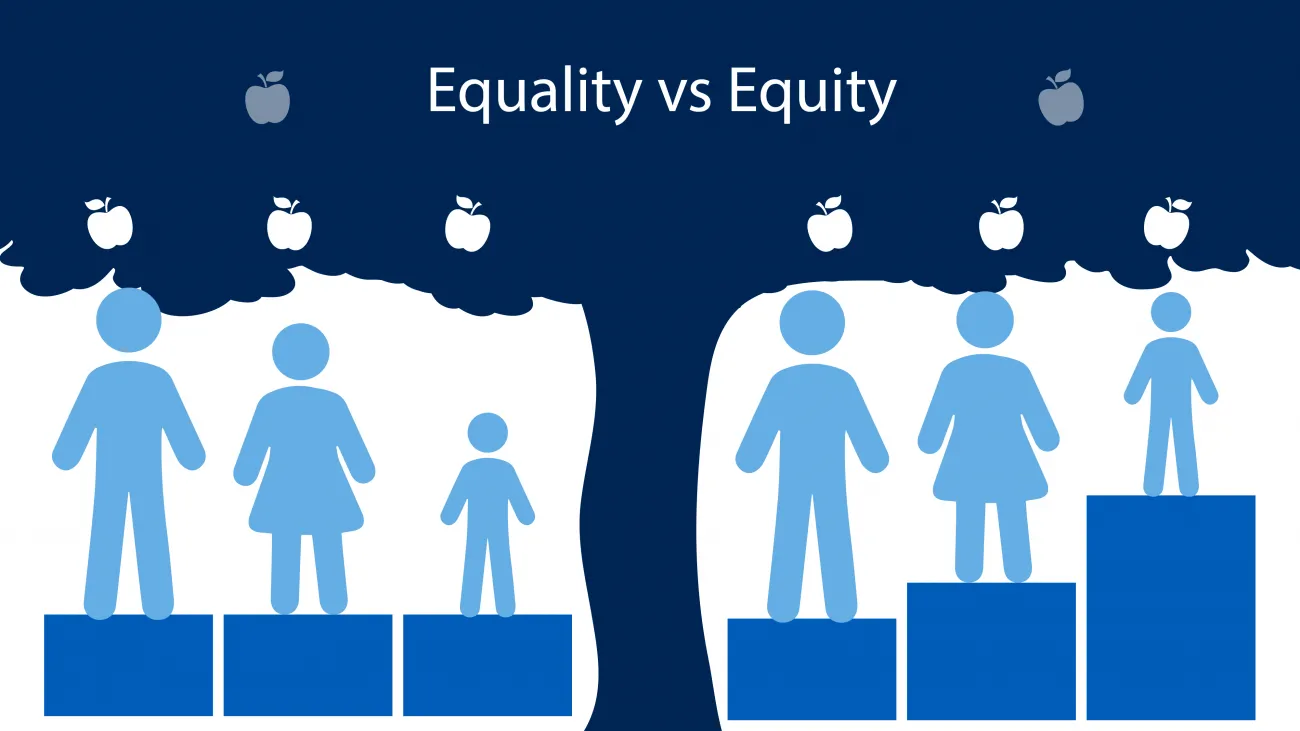
It might seem obvious, but it’s easy to think we’re working towards health equity when our efforts are focused on equality. It’s essential to be clear about what you’re pursuing.
The Centers for Disease Control and Prevention (CDC) says that health equity is achieved when every person has the opportunity to attain their “full health potential and no one is disadvantaged from achieving this potential because of social position or other socially determined circumstances.”
And while health equity and health equality both focus on improving health outcomes and increasing access for underserved populations and marginalized groups, there are distinct differences.
Health equality is when everyone has the same opportunities, quality of care, and access to services. Examples of equality efforts include a clinician ensuring that every patient is asked the same health assessment questions or giving every patient the same educational information, or providing every patient with the same disease the same suggestions for improving symptoms.
Health equity, however, strives to end biases and barriers that lead to health inequities. Examples of equitable efforts include extending clinic hours to evenings, late-night, or weekends to make care accessible for people who work various schedules or provide mobile health screenings and low-cost services where groups that have been economically and/or socially marginalized live and work.
Which are you pursuing, health equality or equity?
How do you know if you’re pursuing health equity versus equality in your health equity strategy? Look carefully at the types of questions raised as part of equity efforts and where outcomes and performance measures are focused. Here are some questions from the American Medical Association’s (AMA) STEPS for Health Systems guide and how whether they orient towards equality or equity.
- Health Equity - Do preventive screening rates, treatment recommendations, or other measures of the quality of our patient care differ by race, ethnicity, and/or language?
- Health Equity - Does everyone in our practice and health system understand how institutionalized racism shapes clinical practice, patients' health outcomes, and the health of the community? How can we better understand or deepen our understanding?
- Health Equality - Do all patients feel equally welcome by our employees and comfortable in our clinic?
- Health Equality - Do all employees feel equally welcome and comfortable at work?
- Health Equity - Do our recruitment and hiring practices consider diversity within our organization?
- Health Equity - Are our recruitment and hiring practices bringing in individuals who represent the patient population we serve?
Both equality and equity are important; however, being clear about how they differ can ensure that your efforts achieve the mission and vision you’ve set.
Fulcrum 2: Health equity analytics and research
While the majority of U.S. hospitals are recording REaL/REaLS data (race, ethnicity, language preference, sexual orientation) in their electronic health record, having the data doesn’t equate to understanding patient needs, perceptions, and barriers to better health.
Advanced healthcare data analytics, artificial intelligence (AI) technologies and additional research are most likely needed. Health equity analytics is foundational to identifying opportunities where targeted interventions (Fulcrum #3) can reduce health inequities. Also, supplementary data sources are useful, incorporating social determinants of health (SDoH), claims, and data outside the clinical encounter, where possible. And, when tools don’t fit the health equity analysis needed, our firm has designed an advanced tool, RTI Rarity™, that forms LSI, a composite index for evaluating data at the granular level from many data sources.
Executing a successful health equity analytics strategy
Conducting primary research through interviews and focus groups can complete the equity picture created with data. Tapping human-centered design techniques, as well as professionals and community leaders who already engage deeply with a cross-section groups of people, can uncover values, beliefs, and patterns that indicate barriers to better health and care.
Exposing assumptions and biases with health equity analytics
Those providing analysis or conducting research must capture their assumptions. Our preconceived notions can get in the way of discovering methods – some very simple and specific – to remove barriers. For example, one Seattle-based health system noticed that patients often arrived for their colonoscopies having not adequately prepared. This creates a poor patient experience and is problematic to the provider regarding opportunities to complete cancer screenings. The analysis uncovered that English-only instructions created a barrier. They started providing materials and classes in the native languages of the persons most affected. This one intervention completely changed the system’s success at delivering cancer screenings.
Using health equity analytics to uncover root causes & opportunities for improvement
Lastly, deploy root cause analysis (RCA), a quality improvement approach to identify the underlying causes of specific incidents. In the Seattle example, clinic staff looked at patterns of patients who needed to have their colonoscopies rescheduled. Also, they talked directly with some patients to determine why they hadn’t prepared. This analysis revealed that patients who spoke two specific languages had literacy barriers to following the pre-procedure instructions.
Fulcrum 3: Targeted health equity interventions
Health equity teams can identify priorities and develop targeted interventions with an improved understanding of people’s health beliefs, needs, and barriers. The Robert Wood Johnson Foundation (RWJF) has an excellent guide that includes suggestions for performing RCA and creating a priority matrix to help narrow where to focus intervention. Then, the team can creatively think of tactics and strategies to address equity gaps.
Ensuring your health equity strategy targets the right groups
It’s important, however, to look beyond interventions that focus solely on patients. RWJF’s Finding Answers literature reviews reported that “50% of health disparity interventions targeted patients, most often with education. Only about 20% of interventions targeted providers, the care team, organizations, or health policy. “ They recommend that interventions look across levels, targeting more than one, when possible. The levels recommended by RWJF include patient, provider, microsystem, organization, community, and policy.
Simplifying a data-driven approach to health equity interventions
Interventions don’t necessarily need to be complicated. Allina Health was also facing challenges with colorectal cancer screenings. Their data-driven approach created interventions that achieved a three percent relative improvement in screening rates. Their interventions included a variety of tools and methods – some more complex or costlier than others:
- Mail patients home testing/screening kits
- Use culturally-tailored education materials, instructions, and FAQ documents
- Employee care guides help patients address barriers, including non-medical challenges
- Social media campaigns engage minorities and languages that their data showed had lower screening rates
And while some teams may focus on disease-, service-, or population-specific interventions, leadership and equity teams approach organizational-level strategies. In December 2021, the National Committee for Quality Assurance (NCQA) launched the Health Equity Accreditation Plus program in cooperation with nine U.S. healthcare organizations. Their framework and five-step process aims to:
- Reduce health disparities
- Align organization and work culture with diversity, equity and inclusion principles
- Partner internally and externally, including workforce recruitment, retention, and development
- Show members, patients, and their communities actions taken to improve health equity
- Demonstrate commitment through NCQA accreditation
The need for health equity intervention on a macro and micro level
As public pressure, value-based care, and regulatory compliance expands and extends a focus on health equity action, interventions at all levels are needed. For example, NCQA adding race and ethnicity stratification for five HEDIS measures in MY2022 demonstrates their commitment to highlight disparities in care and move towards holding plans accountable for implementing interventions to reduce health disparities.
More tips for improving your health equity strategy
In Part 2 of this article series, we’ll explore four more “fulcrum points” to increase momentum towards health equity improvement. These will look at operations, performance, reporting, and quality improvement.
Harness end-to-end health equity support
Our team provides expertise across the health equity continuum, from data and research strategies to analytics tools and services to programmatic design and quality improvement. We take a tailored approach built on best practices but are as unique as your culture and the people you serve.
Learn more about RTI Health Advance, where we’re illuminating the way toward equitable health.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.