We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Healthcare Quality Improvement: How Well Are We Addressing Health Disparities And Inequitable Care?
Healthcare quality improvement progress in achieving equitable care: Where are we now?
Twenty-plus years ago, the Institute of Medicine’s report “Crossing the Quality Chasm” positioned equity alongside five other domains of healthcare quality -- safe, effective, patient-centered, timely, and efficient. Here we explore progress made to address inequities of care through healthcare quality improvement and outline various priorities for 2022 and beyond.
COVID-19 pandemic highlights persistent health disparities
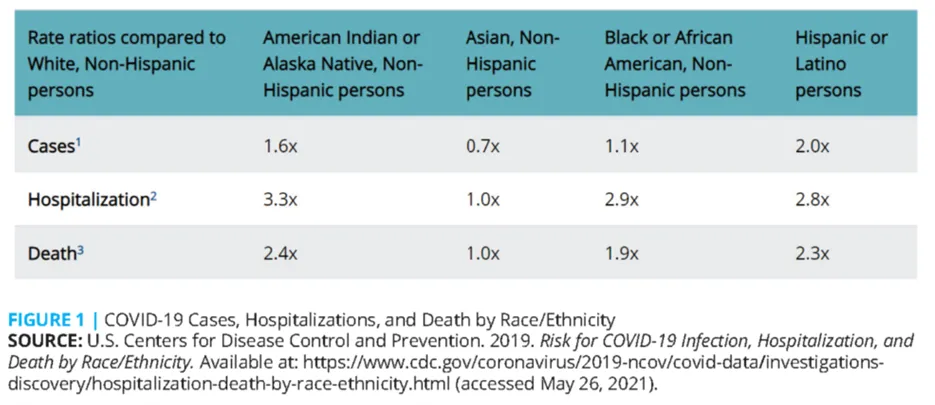
The COVID-19 pandemic confirmed that there are still persistent and stark inequities in care. The U.S. Centers for Disease Control and Prevention (CDC) published health disparities research demonstrating that, compared to Whites, Non-Hispanic persons, Black, Indigenous, and People of Color (BIPOC) faced a greater number of cases, hospitalizations, and deaths, as shown in Figure 1 below.
Current healthcare quality improvement initiatives with a focus on equitable health
In a recent editorial in BMJ, Dr. Lisa Hirschhorn and colleagues suggested three potential outcomes of healthcare quality improvement strategies on health equity:
1. Equality in improvement for all, but there remain equity gaps
2. Decreasing equity gaps
3. Widening equity gaps
While evidence varies on the Impact of healthcare quality improvement strategies, policies, and initiatives to reduce inequity in care, there are clear areas of progress as well as critical improvements to maintain momentum toward desired outcomes. Figure 2 maps many of the current healthcare quality improvement strategies and whether they are provider-focused, payer-focused, or include both payers and providers.
| QI Area | Provider-Focused | Payer-Focused | Payer & Provider-Focused |
|---|---|---|---|
| Data Collection |
HITECH Act PCMH |
HEDIS |
CMMI SDoH PICORI REaL Data HRET Toolkit |
| Analysis & Evidence | HRSA | HEDIS |
PICORI REaL Data |
| Root Causes |
SDoH PICORI |
||
| Solutions & Strategies |
PCMH ACO CHC CHW |
ACA Section 115 Waivers |
CMMI SDoH CBO CM/DM |
| Performance Measurement & Reporting |
ACO HRSA |
HEDIS | CMMI |
| Cost, Payment, Financial Rewards |
HITECH Act ACO HRSA |
ACA Section 115 Waivers |
CMMI CBO |
Sample healthcare quality improvement strategies addressing health equity successfully
Health equity research and development emerged two decades ago, asking if health disparities exist. Today, the discipline has already uncovered evidence about why they exist, as well as what strategies are having an impact and reducing inequities in care. Here is a sample of successful health equity initiatives:
Data collection
Published research highlights recent improvements in structured data collection and analytical approaches to integrate race and ethnicity data into quality measures. Additionally, health plans that have implemented equity-focused initiatives have documented reductions in health disparities and improvements in overall care quality.
Targeted population communication
Payer Health Net used patient-level, provider, and public mapping data to design an intervention to improve cervical cancer screening rates among Chinese members ages 24 to 64. They had found that this group of members historically experienced lower rates. The health plan organized an education campaign on the importance of cervical cancer screening, developing materials in English and Mandarin. More than half of the patients in the campaign scheduled a screening appointment, resulting in a four percent increase in cervical cancer screening rates for its Mandarin-speaking Chinese members.
Another example is Kaiser Permanente. They reduced health disparity in hypertension control between Black and White patients by 71 percent. The program focused on achieving reliable and sustainable collection of race, ethnicity, and language data; implementing proven population care management programs; and changing team-based approaches to be more culturally sensitive.
Language assistance
Language services, when systematically implemented, are touted as one of the most robust interventions for improving equity. Known as Culturally and Linguistically Appropriate Services in Health Care, or CLAS standards, they guide how organizations can best address the increasingly diverse communities and fulfill the Federal mandates for language assistance.
Community health centers
The Health Resources and Services Administration (HRSA) Health Disparities Collaboratives was the largest multi-site quality improvement effort focused on underserved populations. This initiative demonstrated improvement in clinical care processes and outcomes for underserved populations. Many centers achieved measurable improvements for patients with heart disease, diabetes, asthma, HIV/AIDS, and other conditions.
Hospitals and affiliated clinics
Robert Wood Johnson Foundation’s (RWJF) Expecting Success program improved care for patients with heart disease in hospital and ambulatory settings, eliminating documented racial or ethnic cardiac care disparities in four of their 10 participating hospitals.
Building trust & cultural humility
In 2018, UnityPoint Health opened its first health clinic offering dedicated services for LGBTQ+ communities. Adopting an approach of cultural humility, they engaged their LGBTQ+ community to understand challenges, barriers, and what the health system could do to serve the community’s needs. From those efforts, UnityPoint established additional clinics, expanding LGBTQ+-inclusive training.
Health equity data
In 2021, Blue Cross Blue Shield of Massachusetts (BCBSMA) launched a set of initiatives to reduce health inequities and improve racial justice. They made charitable investments in local organizations, convened a Health Equity Council, and created a comprehensive approach to solicit and collect REaL data from all BCBSMA members.
Advancing health equity by addressing health disparities in 2022 and beyond
Despite these successful initiatives, health disparities remain a common marker of poor health system performance, and daunting challenges remain in improving health equity. According to Dr. Ernest Moy, lead staff for the AHRQ’s National Healthcare Disparities Report, "If we say we can improve quality, but only for some, that others will be left out, Americans would say that's [an] unacceptable direction to go."
Currently, there are several significant trends and initiatives focused on the next phase of improving health equity:
CMS priorities
Dr. Meena Seshamani, the current CMS Director, participated in a webinar to share its health equity priorities. As she stated, “The health care system can wait no longer to rectify the long-standing health inequities that adversely affect people in the United States…”
“For the Centers for Medicare & Medicaid Services (CMS), health equity means the attainment of the highest level of health for all people, whereby every person has a fair and just opportunity to attain their optimal health regardless of race, ethnicity, disability, sexual orientation, gender identity, socioeconomic status, geography, preferred language, or other factors that affect access to care and health outcomes.”
Medicare’s vision for health equity is two-fold: improving operations and implementing policies that advance health equity.
Language and access
CMS has proposed requiring multi-language inserts in all required Medicare Advantage plan communications that direct people to free language and translation services. Also, they are proposing new metrics to assess how provider organizations implement operational changes needed to promote health equity.
Telemedicine and digital health solutions
CMS is working to address geographic barriers to care by permanently allowing people in their homes to access telehealth services, including audio-only telephone calls, for behavioral health conditions.
Cost
Low-income older adults and adults with disabilities can receive access to financial assistance with premiums and cost-sharing through the Medicare Savings Programs. While these programs provide healthcare access for millions of Americans, only about half of those who are eligible for these benefits enroll. In 2021, Medicare increased efforts to communicate these programs broadly, increasing enrollment significantly.
Data
Completeness of race and ethnicity member data among health plans remains low. According to HEDIS data in 2019, 76 percent of commercial health plans reported incomplete race data, and 94 percent reported incomplete ethnicity data for more than 50 percent of their members.
Medicaid and Medicare plans fared better, with 50 percent of Medicaid and 26 percent of Medicare plans reporting incomplete race, and 70 percent of Medicaid and 60 percent of Medicare plans reporting incomplete ethnicity. However, CMS is pushing to improve data access and quality. CMS is now including race and ethnicity as optional questions as part of Medicare Advantage enrollment.
Equity health equity measurement and reward
Medicare-Medicaid dual eligibility has shown to be an important predictor of both social risk and adverse health outcomes. CMS is seeking input on how best to stratify quality measures in hospital and skilled nursing facilities by markers of social risk, as well as creating a new health equity index to identify and reward Medicare Advantage and Part D plans.
ACO, rural care, and resident positions: Medicare is exploring new policies to support accountable care organizations in rural and other underserved communities. Also, CMS is expanding funding for medical residency positions, prioritizing hospitals that serve rural and other underserved areas.
NCQA and HEDIS priorities
The National Committee for Quality Assurance (NCQA) has implemented data stratification by race and ethnicity in the Healthcare Effectiveness Data and Information Set (HEDIS). To this end, NCQA added race and ethnicity stratification for five HEDIS measures in measurement year 2022.
The five measures span several key areas with known health disparities, including colorectal cancer screening, controlling high blood pressure, hemoglobin A1C control for patients with diabetes; prenatal and postpartum care; and child and adolescent well-care visits. Temporarily, plans may use indirect data collection methods, such as geographic imputation, to report the race and ethnicity stratifications.
The current timeline earmarks measurement year 2023 for up to 10 measures, using direct and indirect data as needed, and up to 15 measures by measurement year 2024 with 80 percent of data through direct sources.
Health plans have voiced a need for support to enact the new measurements, including the feasibility of collecting self-reported race and ethnicity data, their capability to implement advanced imputation methods, and the need for a flexible timeline to allow plans to collect better direct data.
Taking next steps to enhance improve healthcare quality through health equity
More equitable healthcare won’t come from a particular payment model, delivery approach, or initiative. It takes leaders to engage the communities where they provide care, commit to the larger programs at the federal and state levels, and take an introspective view of their own organizations, deciding how they can improve care quality for all by ensuring equitable care for those who are often overlooked.
Achieve more equitable care for all patient populations
Our team supports healthcare organizations in identifying and addressing the causes of health inequities. We create practical and effective solutions through data analytics, proprietary artificial intelligence and machine learning platforms, and proven expertise.
Learn more about RTI Health Equity Consulting and connect with a health equity consultant today.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.