We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Preventive Measures: Applying Value-Based Care To Behavioral Health
Despite the rapid expansion and adoption of telehealth during the pandemic, lack of access to behavioral healthcare in the US persists. According to the 2023 State of Mental Health in America report, over half of adults with a mental health condition and over 93% of adults with a substance use condition reported receiving no treatment. Youth numbers are similarly troubling, where just under 60% of youth with depression reported receiving no care.
Cost of care is a primary barrier: over 40% of adults forgoing care did so because they could not afford it. This financial barrier to care is echoed in a recent Kaiser Family Foundation survey of women who cited cost as a barrier to mental healthcare, along with lack of provider availability.
Connecting Americans to early and affordable care for their mental health and substance-use conditions can prevent a worsening of symptoms, interrupt negative impacts to daily functioning, and promote overall health and wellness. The bright spot is that the healthcare system can leverage an existing framework for early treatment of chronic conditions: the preventive health benefit available through health insurance plans.
Getting ahead of behavioral health conditions
Heart disease is a leading cause of death in the US, driving $216 billion in healthcare costs and $147 billion in lost productivity, and can largely be addressed with early identification and preventive interventions. Major depressive disorder alone has a staggering impact on the US, with an estimated economic toll of $326 billion and a reduction in quality of life of 2.7 million disability-adjusted-life years. As with heart disease, much of the burden from major depression could also be reduced with preventive care and early interventions. Sitting at the intersection of healthcare delivery, provider engagement, and development of healthcare benefits, commercial health payers are in a unique position to unlock the potential of expanded behavioral health preventive benefits by focusing on 3 actionable steps:
- Promote emotional well-being, improve quality of life, and help people thrive
- Reduce stigma associated with behavioral health conditions by normalizing and treating behavioral health conditions as we treat physical health conditions
- Reinforce VBC through early identification, right-sized interventions for patients, and reduction in higher-cost services
The state of preventive benefits
Preventive health and associated preventive benefits under medical health plans are fundamental aspects of primary care and quality healthcare in the US. Preventive services focus on early detection and intervention to reduce an individual's risk of developing a chronic condition, such as hypertension or diabetes, minimizing progressive negative impacts from a chronic physical condition, promoting longevity, and reducing healthcare costs.
Commercial health plans establish preventive health benefits largely on the evidence-based recommendations from entities such as the U.S. Preventive Services Task Force (USPSTF), the Centers for Disease Control and Prevention (CDC), and the Women's Preventive Services Initiative (WPSI). Services covered under the preventive benefit are at no cost to the individual when delivered by an in-network provider, which creates a low barrier to essential care.
Preventive benefits cover screening for anxiety, depression, and substance use in adults, screening for anxiety in children aged 8 and over, and depression screening for children aged 12 and over. Universal behavioral health screenings identify emerging signs of depression and anxiety, such as changes in mood, increased worry, sleep disruption, and decreased enjoyment in activities. The discussion with the pediatrician or primary care provider about recommended behavioral health treatment is also covered under the preventive benefit.
How preventive benefits fall short for behavioral health
Unlike medications to help quit smoking or intensive behavioral counseling for adults at risk of developing cardiovascular disease, the counseling provided by a behavioral health provider to address early signs of depression and anxiety are not covered under the standard preventive benefit. Outpatient behavioral health counseling is covered under the specialist benefit and typically involves a co-pay that can be $20-40 per session with an in-network provider.
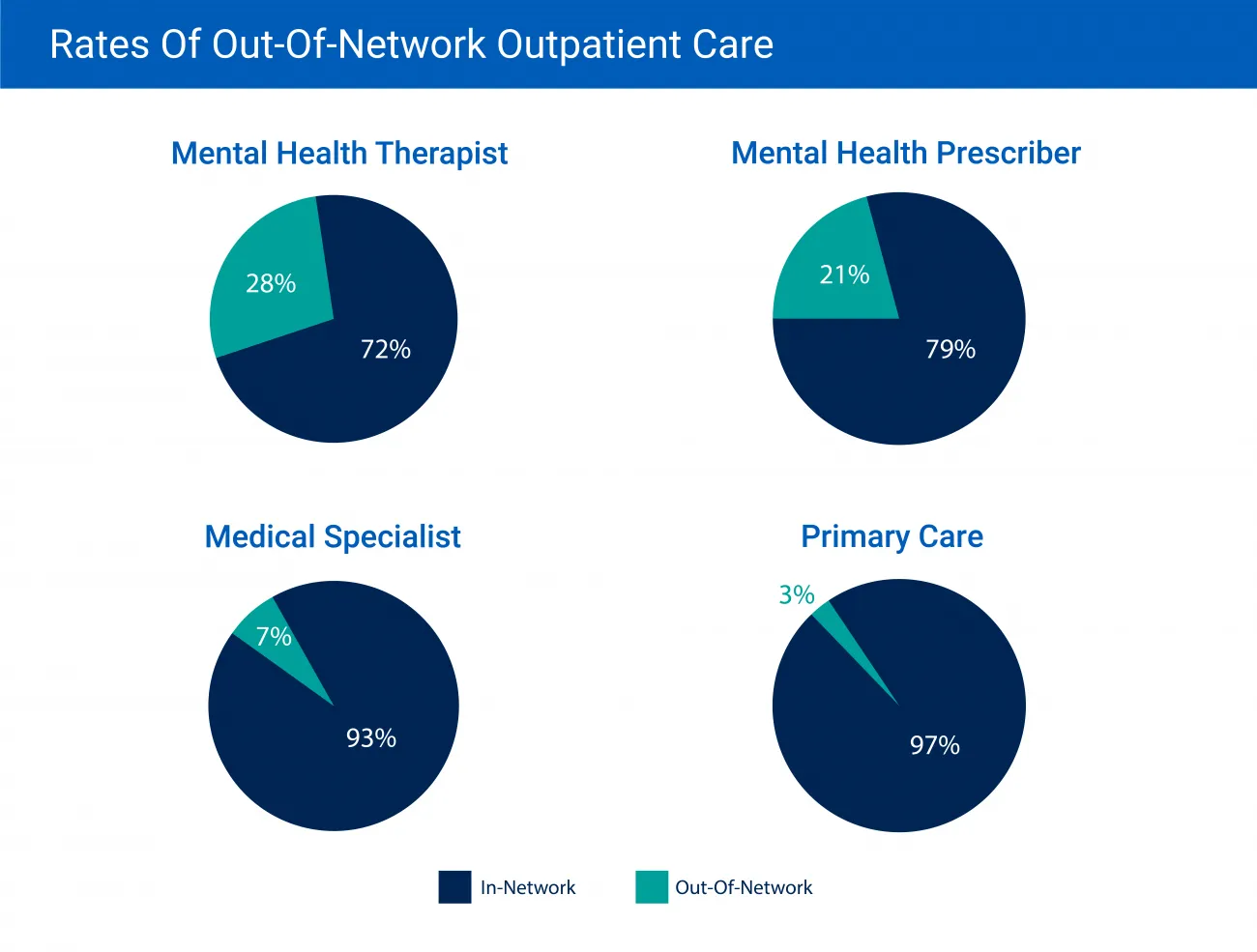
One series of short-term counseling for mild anxiety and depression can range from 6 to 20 sessions, creating a financial impact between $120 to $800. This out-of-pocket cost is incurred after having met a health plan's deductible, averaging $1,644 for an individual on an employer-sponsored plan to over $4,000 for a marketplace Silver plan. Costs frequently soar even higher as behavioral health office visits are more than 5 times likely to be with an out-of-network provider, compared to medical/surgical primary care office visits, according to a 2019 report. This could be due to:
- The shortage of behavioral health providers
- Inability to find a provider meeting the cultural needs of historically marginalized BIPOC individuals
- Providers opting to not accept insurance due to health plan administrative hurdles and lower reimbursement rates
Health plan structures can be a barrier
Commercial health plan benefit design and claim processing systems may not support behavioral health providers in treating and receiving compensation for early preventive behavioral health interventions. Providers must include a valid behavioral health diagnosis on their claims, meaning that coverage is tied to a person already meeting clinical criteria for a behavioral health diagnosis. Expanding the scope of defined preventive benefits will create more holistic coverage, supporting individuals with mild conditions in addition to those needing intensive services for moderate and severe mental illness (SMI). Creating a more robust continuum of benefits for behavioral health conditions is endorsed by Mental Health America, the National Association of State Mental Health Program Directors, and policy institutes, such as the Center for American Progress:
“In the same way that a patient can be screened for complications by their primary care provider—as well as specialists, such as gynecologists, ophthalmologists, and cardiologists—patients should be able to see behavioral health providers for early treatment or maintenance of concerns or complications, even if those sessions do not result in diagnoses."
Early behavioral healthcare is value-based care
Just like early prevention efforts lessen the effects of chronic physical health conditions, early treatments for mental health and substance use conditions make good clinical and economic sense. Of the 46% of Americans who will develop a mental health condition in their lives, about half will have developed that condition by the age of 14, underscoring the importance of early detection and intervention. Research by the Healthy Brains Global Initiative found prevention and early intervention the top area of unmet need in addressing anxiety and depression in youth, followed by investment in school and community-based programs. Beyond improving health and wellness, investing in services for youth when they start to develop behavioral health conditions can return real savings to the community, where $1 in prevention can yield $2-10 in savings by avoiding downstream costs associated with juvenile justice, costly healthcare, and decreased productivity.
The total cost of care for individuals with behavioral health diagnoses is significantly higher compared to those without a behavioral health diagnosis. According to a 2020 study by Milliman, individuals with behavioral health conditions have up to 6.2 times higher medical/surgical healthcare costs than those without a behavioral health condition. Further, the study uncovered that the elevated healthcare costs were for people with lower levels of behavioral health conditions, according to psychiatrist and behavioral health expert, Dr. Henry Harbin. In an interview with the American Journal of Managed Care, Dr. Harbin noted:
“As you look at the report that Milliman did, it's interesting that the majority of these costs are driven by people with mild to moderate mental health or substance abuse problems. There's commonly a misconception it's the patients with more severe mental illnesses like psychosis or schizophrenia that are the ones that drive these costs. That's not true."
Commercial health plans that invest in removing member cost sharing for outpatient behavioral health visits and create benefits for early, preventive care can see returns through improved member well-being and reduced healthcare costs. Recent research on the impact of providing outpatient behavioral health treatment demonstrated total cost of care savings of over $3,000 per person over 2 years, where savings started after just 3 behavioral health outpatient visits.
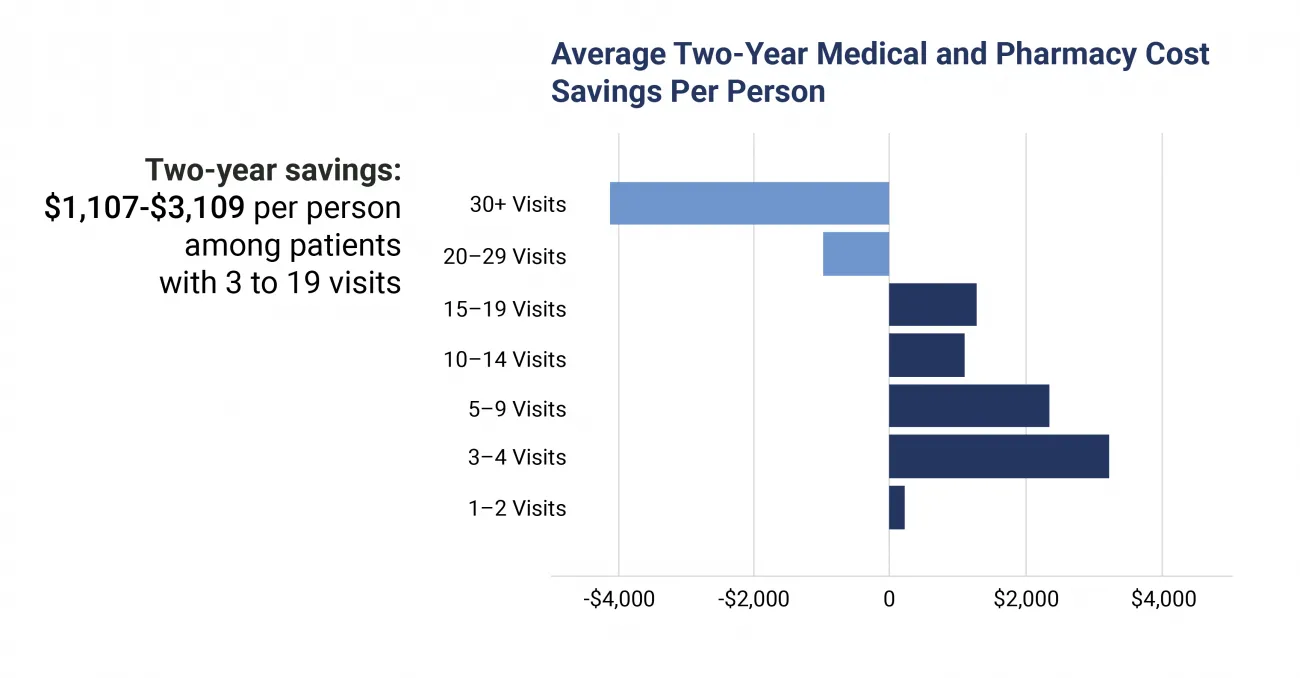
Fig. 2 Behavioral Health Savings via Evernorth
Though value-based care (VBC) for behavioral health may have hurdles, it can be a way to champion and demonstrate the value of early preventive behavioral healthcare. Health plans can partner with and incentivize primary care, OB/GYN, oncology providers, and other clinical specialties to increase adoption of behavioral health integration. To overcome the costs associated with co-located behavioral health services, payer-provider partnerships can leverage technology and evidence-based pathways to early treatment, such as:
- Digital behavioral health solution platform capabilities
- Patient-reported outcome measurement
- Digital interventions
- Self-guided computerized cognitive behavior therapy content
Step closer to health equity with early intervention
Upstream identification and support for behavioral health conditions can bring care to BIPOC communities which have long faced barriers to behavioral healthcare access, such as racism, discrimination, and structural inequities. Here are steps health payers can take to increase early treatment:
- Collaboration and investment with providers to implement systematic, universally-recommended behavioral health screening can promote increased and equitable access to care, especially paired with no-cost preventive behavioral health benefits
- Actively engage the community and plan members to understand their lived experience and identify behavioral health needs to inform payer decision making and action
- Partner and contract with digital solutions and provider groups with services and counseling for BIPOC and LGBTQIA+ individuals, making certain these resources are visible to members via multiple channels, such as provider directories, web content, and member communications
- Reimburse for evidence-based/community-based programs and interventions, which can help reduce disparities in preventable hospitalizations for individuals with physical and behavioral health conditions
Recent developments
The wheels of change move slowly, though some progress is underway. Signs that the healthcare system is removing barriers and elevating early behavioral health treatment include:
- Commercial health insurance carrier Cigna broke new territory in 2021 when it partnered with Ginger to create the industry-first, in-network benefit coverage for certified behavioral health coaches who can provide early support for behavioral health concerns. This move expands the types of behavioral health providers available to members, relieving some pressure on the short supply of behavioral health providers, and helps payers meet increased demand for care from expanding coverage for early interventions.
- In 2021, New Mexico's Health Care Affordability Fund eliminated copays and other cost sharing for behavioral health services for residents covered under fully-insured plans.
- Covered California, California's health insurance marketplace, aimed to make access to behavioral healthcare more affordable by not charging for the first 3 non-preventive office visits including behavioral health visits and offering “first-dollar" plans where specialist services like behavioral health are not subject to the plan's deductible.
- The US House Committee on Veteran Affairs introduced the Reduce and Eliminate Mental Health Outpatient Veteran Copays Act or REMOVE Act, to reduce financials barriers to getting behavioral healthcare by removing copays for the first 3 behavioral health appointments each year.
Champion early behavioral health care
Commercial health payers are committing to providing their members with easier access to behavioral healthcare and are taking steps to reduce healthcare disparities. Commitment to change needs to be paired with data and evidence to inform decision making. Through modeling, advanced healthcare data analytics, and advisory services, RTI Health Advance can provide your organization with the evidence and insights to inform benefit design, behavioral health programing, and value-based model success.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.