We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Unwinding From The Public Health Emergency: Medicaid Redetermination & Beyond
State Medicaid directors and their teams have an enormous initiative ahead of them to unwind policies and programs that were instituted as part of the COVID-19 public health emergency (PHE). The Families First Coronavirus Response Act (FFCRA) included a requirement that Medicaid programs maintain continuous coverage until the PHE ends, which we now know will be May 11, 2023, in exchange for enhanced federal funding. While the program has ensured healthcare coverage for previously and newly eligible adults and children for nearly three years, their enrollment could end soon.
After being extended for the twelfth time in January 2023, state Medicaid offices have been preparing for a for a complex and critical next phase. How well these overburdened teams unwind their state programs and policies will affect the health and care for millions of Americans; many who had no healthcare coverage before the pandemic.
Medicaid and CHIP enrollment extended throughout the public health emergency
As shown in Figure 1, according to KFF, total Medicaid and CHIP enrollment grew by 26.3% to reach 90 million by July 2022. It was an increase of 18.7 million Americans who had coverage because of the continuation requirement or were newly eligible due to financial need or Medicaid expansion in their state. KFF also estimates that between five and 14 million people will lose their Medicaid coverage once the PHE ends. HHS estimates that that up to 15 million people could be disenrolled in the first 12 months after the PHE ends, including 6.8 million who may still be eligible depending on how each state prioritizes renewals.
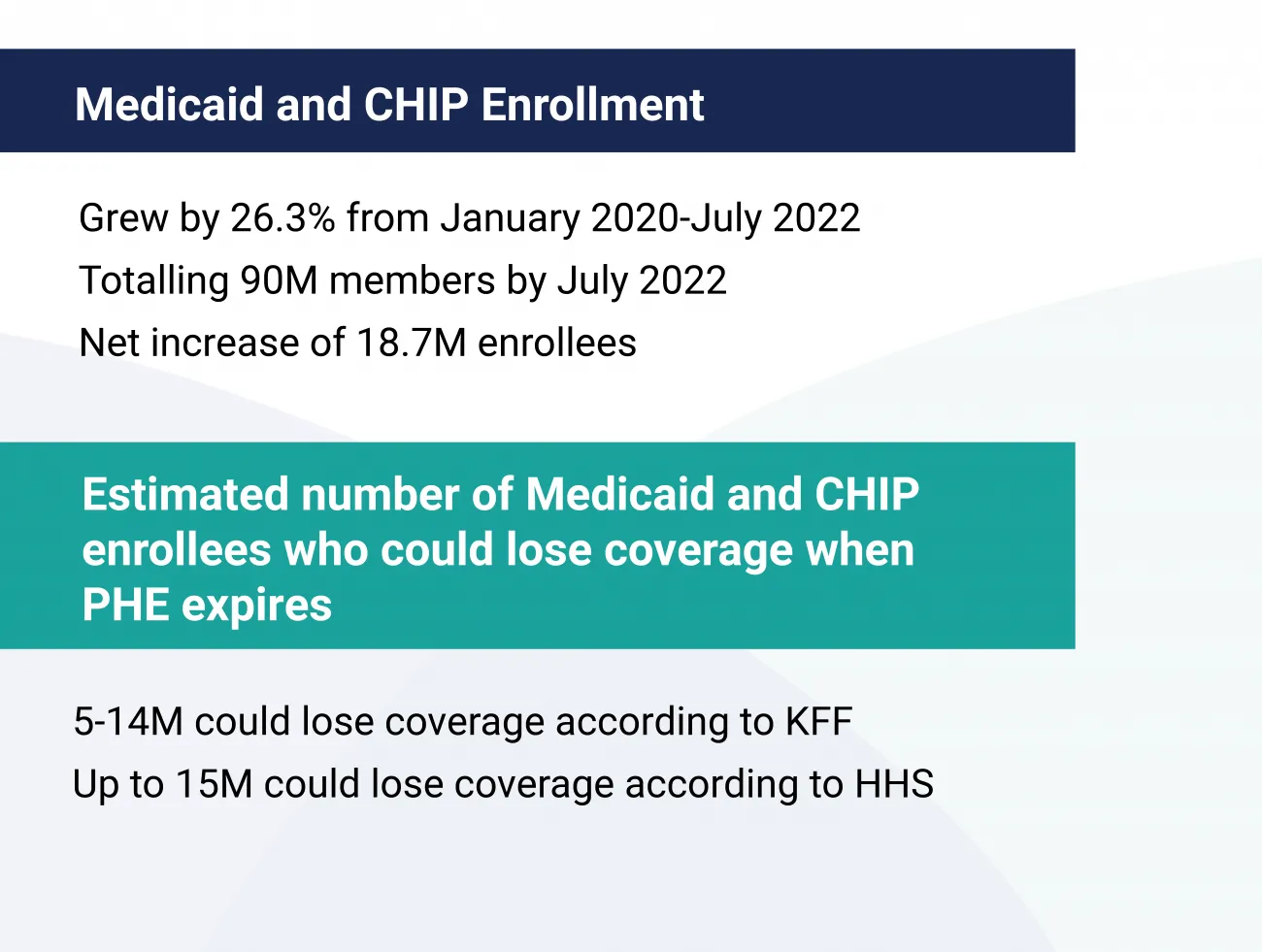
Figure 1: Estimates on changes to Medicaid and CHIP enrollment when the PHE ends
When the PHE ends, what will happen to millions of adults and children currently covered?
Once the PHE ends, states will need to address carry out four critical projects.
- First, they must determine eligibility for everyone who has continuous coverage since the PHE began. Some people may no longer be eligible due to income thresholds or their state's rules.
- Second, states will need to re-enroll those who are eligible.
- Third, states will need to educate those who are no longer eligible on alternatives like the ACA exchanges, accountable care arrangements or other coverage.
- Lastly, Medicaid and CHIP agencies will need to resume routine operations – initiating renewals within 12 months and completing renewals within 15 months.
Additionally, they will have only four months after the PHE ends to resume timely processing of all applications, including new ones received during the unwinding period. They will still be required to meet standards for renewals, verifications, applications and program oversight.
Despite a special enrollment period, it will be a challenging transition
CMS recently announced a special enrollment period for Affordable Care Act coverage for consumers who no longer qualify for Medicaid. This period begins March 31, 2023. It's estimated that nearly 18 million people will be at risk for becoming uninsured.
Because of the moving deadline and the scale of the unwinding, many people enrolled in Medicaid or CHIP are vulnerable to losing coverage because they aren't aware that, after nearly three years, things will revert to pre-pandemic processes. Plus, when the US presidential election is held in 2024, its outcome will influence how states expand or decrease coverage or change their eligibility requirements.
Research by the Urban Institute found that 62% of adults who have Medicaid coverage themselves or for a family member are unaware that Medicaid eligibility redeterminations and renewals will be restarting in the near future. Of those people who enrolled during or after March 2020, 56.5% have heard nothing about eligibility and renewal actions they will need to take. Georgetown University's Health Policy Institute conducted in-depth interviews with 49 enrollees and found that most were not concerned or wondering about reenrollment.
About 50% of those who were aware of the upcoming changes have received a notification from their state agency or health plan. However, the largest source of information (34%) came from the media, including social media. Without proactive and accessible education and communication with Medicaid and CHIP members, millions will unwittingly lose their healthcare coverage.
What does the Medicaid unwinding entail?
Related to eligibility and enrollment, there are a number of key undertakings for state Medicaid offices. An interactive tracker, hosted by Georgetown University, gives a real-time view of what each state has prepared as part of their unwinding. Most have a long way to go to be prepare for the end of the PHE.
Conducted in January 2022, a KFF survey revealed that a little more than 50% of states had created a plan for how they would prioritize renewals. Most were planning to complete renewals in 12 months and some had not created a timeline yet. As of November 2022, 32 states had shared their plan publicly.
During a recent webinar hosted by KFF, the National Association of Medicaid Directors (NAMD), and Health Management Administrators (HMA) the unwinding of programs and policies due to the PHE was the number one concern of Medicaid and MCO leaders.
Directors from Massachusetts and Indiana shared the challenges they are facing, including workforce shortages, many priorities spreading current staff thin, and that many pre-pandemic priorities were postponed like long term services and support (LTSS) and home health programs.
There are a number of milestones states need to achieve to ensure that all enrollees are aware of the coming changes as shown in Figure 2.
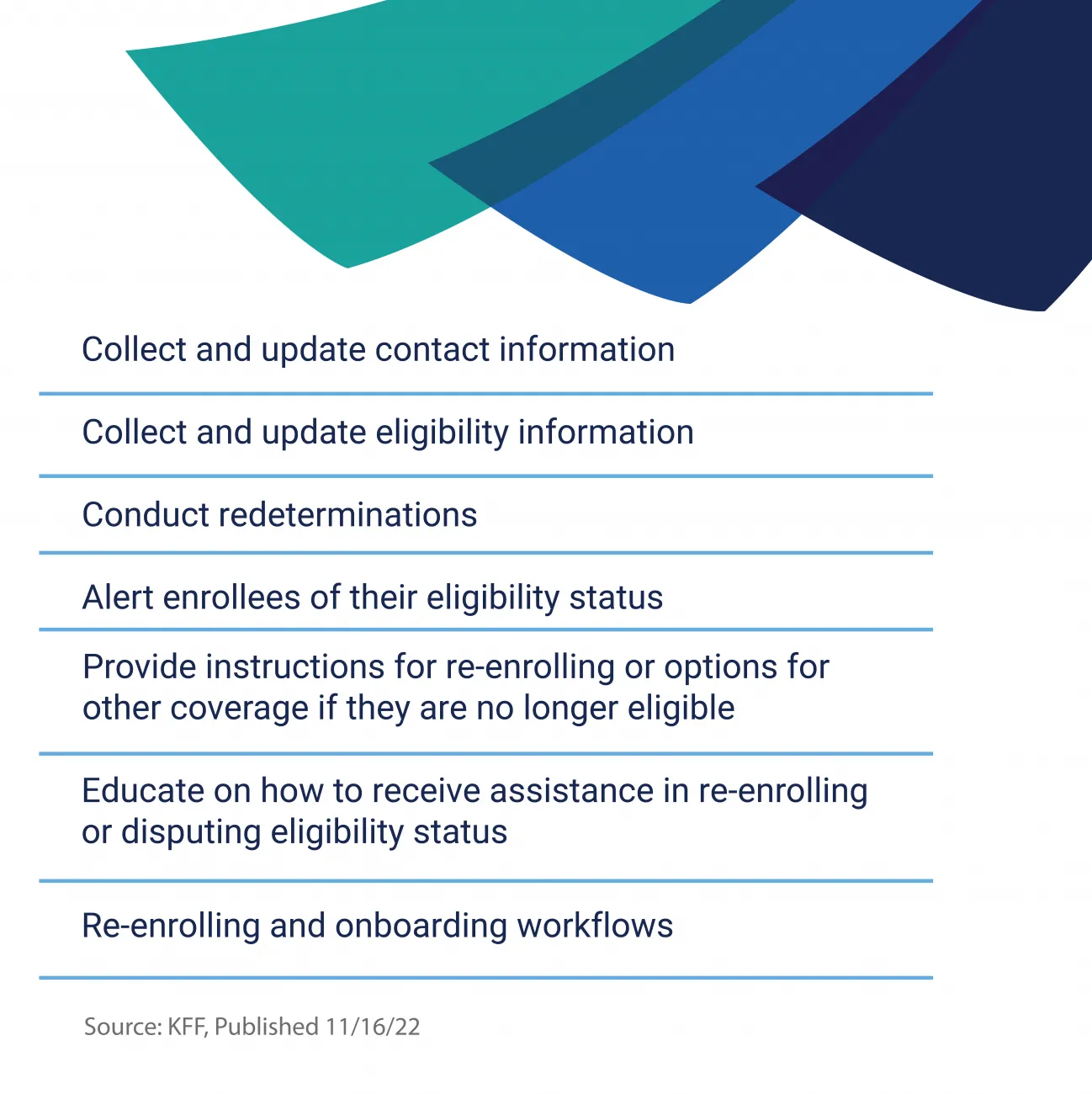
Figure 2: Medicaid unwinding tasks to ensure a smooth transition for members
Industry organizations request support to streamline unwinding
Organizations like the NAMD are engaging CMS and congress to make the unwinding less burdensome for enrollees and their own short-staffed departments. They've called for a longer advance notice (120 days instead of 60 days) of when the PHE will end. They've asked for certainties around deadlines and financial resources and that the underlying Medicaid eligibility rules will not change throughout the redetermination period. Calling the uncertainty around the PHE untenable, NAMD's board has asked for greater support to streamline the renewal process. The Alliance of Community Health Plans (ACHP) offered five recommendations for CMS, including more flexibility in legal restrictions on communication with members.
Strategies states can take to streamline the unwinding
These are a few proactive steps that the industry can take to ensure enrollees are well-supported through the unwinding. There are also other ways agencies can support a smooth transition.
Ramp up "ex parte" renewals
One way that organizations can support streamlining renewal processes is to share data sources that can fill the gaps in information needed to determine eligibility. Complete administrative, or ex parte, renewals allow states to pull in data before sending the renewal form or asking enrollees for additional documentation. With greater access to data, more states could process ex parte renewals. Currently, only 11 states report completing 50% or more of renewals using ex parte processes.
Offer omnichannel data capture
Not enough states offer multiple channels for submitting required information or documents. Most states accept information by mail and in person, however, only 39 states offer phone submissions and less than half of states offer online submissions.
Provide Medicaid and CHIP information in multiple languages, accessibility options
Analysis of state Medicaid websites found that even though most states do offer the online application landing page or PDF application in more than one language, it's typically Spanish. Also, most states provide only basic information on how to access reasonable modifications and teletypewriter (TTY) numbers. Even fewer states provide details on how to access applications in large print or Braille provide options for accessing American Sign Language (ASL) interpreters. However, some states are addressing this concern: In California, their Department of Health Care Services published their PHE unwinding plan that included communication outreach toolkits for Coverage Ambassadors to use when engaging members. It includes information translated in all 19 Medi-Cal Threshold Languages.
Pay attention to health equity issues and areas of concern
A guide published by State Health and Value Strategies—a program of the Robert Wood Johnson—gives salient recommendations and resources for managing the unwinding. They pay particular attention to the health equity risks involved, "The volume of eligibility redeterminations is unprecedented, and there are significant equity implications—transitions between Medicaid and the Marketplace are likely to disproportionately impact people of color, as Black and Latino(a) individuals are significantly overrepresented in Medicaid and CHIP programs."
Partner with MCOs, providers, and community organizations on data and outreach
Ten percent of Medicaid enrollees had moved intra-state in 2020. And, with eviction moratoriums ending in 2021, more moves occurred. This makes maintaining accurate contact information and sending timely notices a challenge. Partnering with community health centers, MCOs and other service organizations can help spread the word and educate enrollees on the changes that are coming. One survey of Medicaid programs found that 39 states had plans to collaborate with fellow state agencies and 32 were partnering with MCOs.
Expanding sources of support during the Medicaid unwinding
RTI Health Advance offers a host of clinical, operational, population health, data science, and digital health experts that can support state agencies through their unwinding preparation and return to pre-pandemic procedures. Whether Medicaid directors need assistance with system readiness artifacts, unwinding data gathering and analysis, renewal redistribution plans, required reporting, or ensuring digital tools are equitable and accessible, we can help. Contact us.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.