We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Omnichannel Digital Solutions Deliver Mental Health Services Across Acuity Levels
Digital health solutions can never replace the value of the relationships built between patients and mental health professionals. The consumerism of healthcare and external factors, including the pandemic, influence the face of care delivery and preferences for ways to engage. Omnichannel digital health solutions offer three levels of support that improve behavioral health access, convenience, and a continuum of care.
As patients and providers unwind from the public health emergency and work to address mental health needs now and into a post-COVID future, what can providers do to align interventions with care delivery channels?
We've developed a matrix that organizes three types of interventions that can be used across levels of acuity via various digital health channels and tools. A payer or provider organization can look at their patient-member needs, IT strengths, and care goals to determine which solution combinations from the matrix meet their care setting.
Digital health acceleration and adoption is pacing to address mental health needs
One of the most profound innovative outcomes from navigating the COVID-19 pandemic is the digital health revolution occurring in mental health care delivery. Virtual care (aka telemedicine or telepsychiatry) now complements or has replaced traditional in-person appointments. Other digital health technologies act as a supplement to or extension of person-to-person intervention and support. These can include synchronous video or audio visits, asynchronous text-based messaging, chatbots, mobile apps, and other channels and methods.
According to KFF, “telehealth visits for outpatient mental health and substance use services went from virtually zero percent in 2019 prior to the COVID-19 pandemic to a peak of 40% in mid-2020 and continued to account for more than a third (36%) of such visits in the six months ending in August 2021." Figure 1 shows that its popularity has been sustainable. The American Psychiatric Association reported that six in 10 Americans would use telehealth services for mental healthcare.
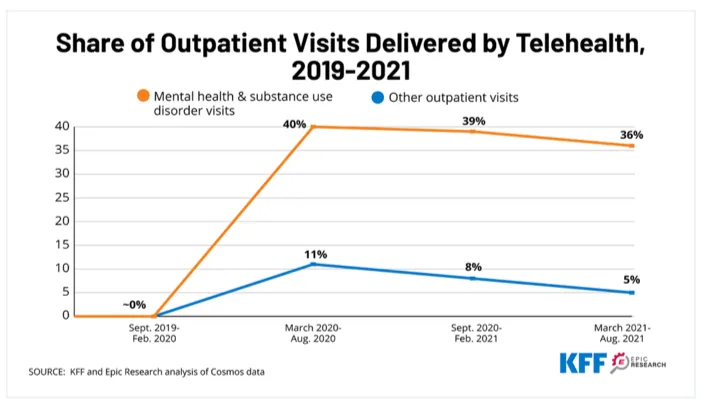
Figure 1: Telehealth usage for mental health and substance use disorder (SUD) vs. all other outpatient visits.
While telemedicine has been found cost-neutral, its helping to fill the gap to provide access to behavioral health services to more people. Additionally, it's improving outcomes. Research published recently in JAMA Psychiatry shared that, “Expanded use of telehealth services during the COVID-19 pandemic was associated with reduced risk of opioid overdoses."
The Harvard Business Review cited a 2020 Veterans Administration study that found video telepsychotherapy was “as effective as in-person office-based care for treating depression and posttraumatic stress disorder. Overall, most published studies show telephonic mental health care is as effective as in-person care in treating depression, anxiety and obsessive compulsive disorder."
Beyond synchronous telemedicine, use of other digital health technologies is ramping up. A Forbes review of the top 10 online therapy services, all leveraging one or more forms of digital health tools, found that 24/7 messaging, text/video/audio messaging were offered across the board with all services in addition to video or audio therapy sessions.
Which digital health technology is appropriate for your patients-members?
It's challenging to gather all the available digital health tools and vet each for each use case, whether in a behavioral health scenario or other specialty. We've assessed available scorecard methodologies for evaluating mobile health apps. Now, we've created a Digital Health Matrix as a framework to answer three questions:
- What level of clinician involvement (intervention strategy) is needed?
- What patient acuity level do we need to treat?
- What digital health tools might best fit combinations of clinician involvement, patient acuity level, and digital tool uncovered by answering the first two questions?
Digital health matrix overview
Figure 2 shows the matrix with digital health tools across columns and three levels of clinician involvement (aka intervention strategy) listed in rows. The green, yellow, red dots indicate if that intersection of digital health tool and level of clinician involvement are appropriate for each acuity level. Green signifies low need, yellow signifies medium, and red indicates the patient has a high acuity level need.
Defining the digital health matrix terminology
The matrix can be used to assess any digital health technologies or tools. However, it's important to have common terms and definitions so that dialogue is productive and the matrix is useful for those discussions.
Type of intervention & level of clinician involvement needed
Complements – This intervention requires the most amount of clinician involvement and monitoring. It supplements in-person or live therapy sessions. This type of intervention cannot be delivered without the clinician.
Extends – This intervention adds new ways to provide therapy and requires less direct clinician involvement and monitoring.
Replaces/Triages – This intervention may replace the clinician or requires little involvement or oversight, relying on the technology. This intervention could also triage mental health needs and connect a patient to a different type of intervention and level of clinician involvement, when or if needed.
Levels of mental health acuity
We referenced the Level of Care Utilization System (LOCUS) for Psychiatric and Addiction Services, simplifying their five-level framework (minimal, low, moderate, serious, extreme) to three levels (low, moderate, high) for this exercise. The acuity levels are not recommended as a clinical indicator of mental health need, but to demonstrate which digital health tools and types of interventions may be more appropriate in lower acuity and more complex clinical cases.
LOCUS considers six areas as evaluation parameters: risk of harm, functional status, co-morbidities, recovery environment (stress), level of support, and engagement and recovery status. For some criteria, like level of support, a lower number indicates more support and available resources.
The matrix could be updated with the five LOCUS levels to conform more closely to the industry standard. For our purposes, acuity levels relate to the LOCUS levels as follows:
- Low – minimal and low
- Moderate - moderate
- High – serious, extreme
Digital health channels and technologies
The matrix highlights eight digital health tools and technologies serving mental health therapeutic areas:
- Telemedicine/virtual care (aka synchronous video/audio)
- Asynchronous video/audio
- Web-based education
- SMS/messaging
- Mobile apps/digital therapeutics
- Wearables/remote patient monitoring (RPM)
- Chatbots, smart devices, and social media
Other technologies could be added to the matrix when assessing scenarios outside those represented in the matrix.
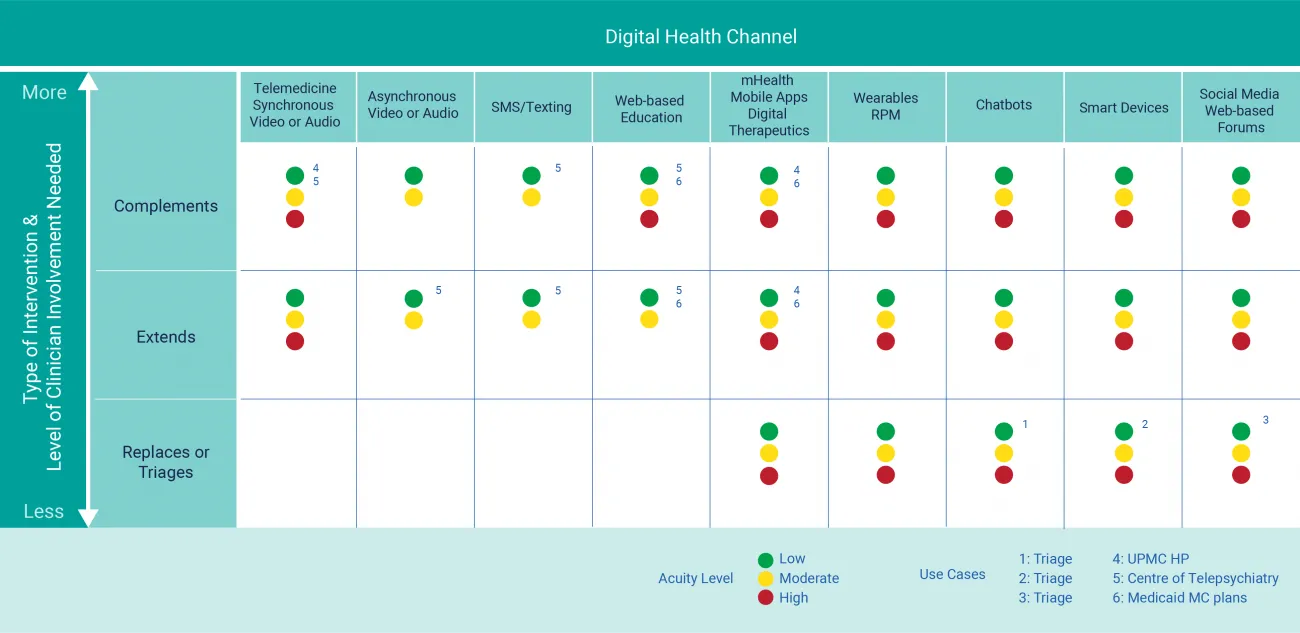
Figure 2: Digital Health Matrix (download the matrix now for reference later)
How to use the digital health matrix
The digital health matrix may be helpful when determining the possible digital health technologies and channels to employ, depending on patient care goals and the patient's level of risk/need.
For example, patients at higher risk levels would not be appropriate for asynchronous video/audio messaging or text. However, chatbots, social media listening or using smart devices could leverage artificial intelligence for tone, words and phrases that might indicate a serious mental health event. Essentially, the digital tool would triage the need and escalate for immediate connection to a clinician. See matrix use cases 1, 2, and 3.
If a provider knows the acuity level being assessed, the matrix may be used to brainstorm the types of digital health tools that might be appropriate based on the level of clinician involvement available. Conversely, a provider can look at the level of clinician involvement available and prioritize which digital health tools might fit staffing as well as patient needs. While the matrix isn't prescriptive, it is valuable in looking at the larger clinical and operational resources available and possible technologies to meet provider goals.
Digital health examples
See matrix use case 4: UPMC Health Plan created RxWell, an evidence-based mobile app for individuals 16 and older, to help members build more healthy lifestyle habits and become more emotionally and physically healthy. It combines health coaching support with provider-endorsed techniques like self-guided exercises and tools to manage stress, anxiety, and depression. Their telehealth service through UPMC, AnywhereCare adds a synchronous video and audio component and provides a convenient and uncomplicated way to obtain a medical evaluation from home.
See matrix use case 5: The Centre of Telepsychiatry uses a stepped care approach, shown in Figure 3. They include self-serve tools, like web-based education and content, virtual care that is blended with in-person formats. They tailor asynchronous and unguided treatment with synchronous real-time treatment depending on the severity of the patient's illness and symptoms.
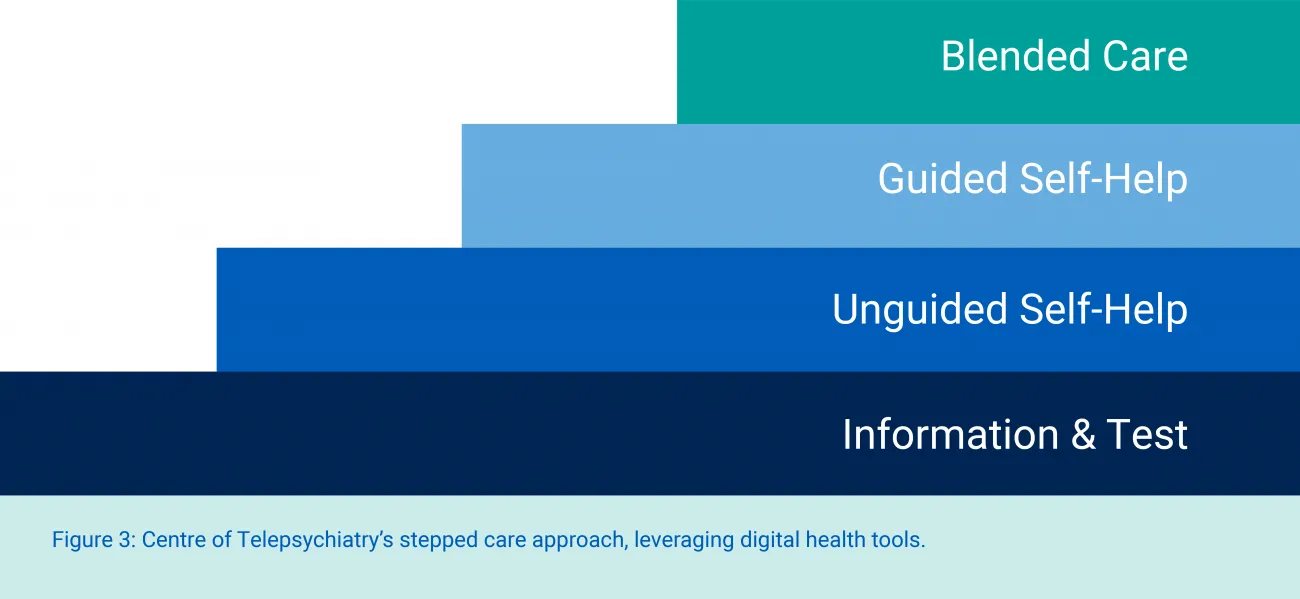
Figure 3: Centre of Telepsychiatry's stepped care approach, leveraging digital health tools.
See matrix use case 6: Medicaid managed care plans are using Livongo's platform, myStrength, to reach out to members who may have unmet behavioral health needs. First-time users answer questions about well-being, social supports, and life experiences. Then, they are directed to a suite of interactive resources based on cognitive behavioral therapy, motivational interviewing, mindfulness, and other evidence-based counseling approaches.
Download our digital health matrix
No matter your clinical and operational goals, a host of robust digital health technologies can supplement and extend your clinician resources. In some instances, technology can give clinicians more time for treatment and more time devoted to patients presenting with more severe acuity by supporting triage or taking over certain tasks altogether.
Try the matrix as a way to brainstorm possibilities. Then contact RTI Health Advance. We provide the clinical, operational, data science, and digital health expertise to assess your goals, recommend robust solutions, and help you implement and achieve performance objectives.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.