We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Redesigning ACO Benchmark Policy
Solving the ACO Benchmark Ratchet
Accountable Care Organization (ACO) programs need to consider alternatives to calculating benchmarks with prior expenditures if the aim is to grow and generate systemic savings. This methodology has a negative impact on high-performing ACOs.
ACO benchmark policy redesigns necessary to drive participation in value-based care models
CMS recently published a goal of involving all Medicare beneficiaries with Parts A and B in an alternative payment model (APM) by 2030. APMs are voluntary programs that rely on inducing provider participation. To date, one of the most documented obstacles to provider participation in APMs is how calculating benchmarks using historic ACO spending artificially lowers future benchmarks for successful ACOs.
A recent paper from the USC-Brookings Schaeffer Initiative for Health Policy proposes a method for decoupling benchmarks from historical expenditures through setting benchmarks administratively. While this paper is geared towards the federal market, the issue described and the proposed solution are relevant to commercial ACOs as well.
How ACO benchmark ratcheting reduces incentives for providers to participate in APMs
An optimal ACO benchmark is high enough to encourage provider participation but low enough to incentivize savings. In most ACO models (including those adopted by CMS and commercial APMs), benchmarks are primarily reset in each performance period according to individual ACO spending in the immediate prior year (or several prior years).
The main criticism of this “rebasing” approach is that savings generated by an ACO in the current performance period are propagated forward to future performance period benchmarks. Successful ACOs become victims of their own success.
There’s another way historic expenditures can influence future ACO benchmarks. Benchmarks are frequently adjusted to align more closely with regional expenditure trends. ACOs with relatively large regional market shares are penalized when they generate savings because their region’s expenditures are highly correlated with their own expenditures.
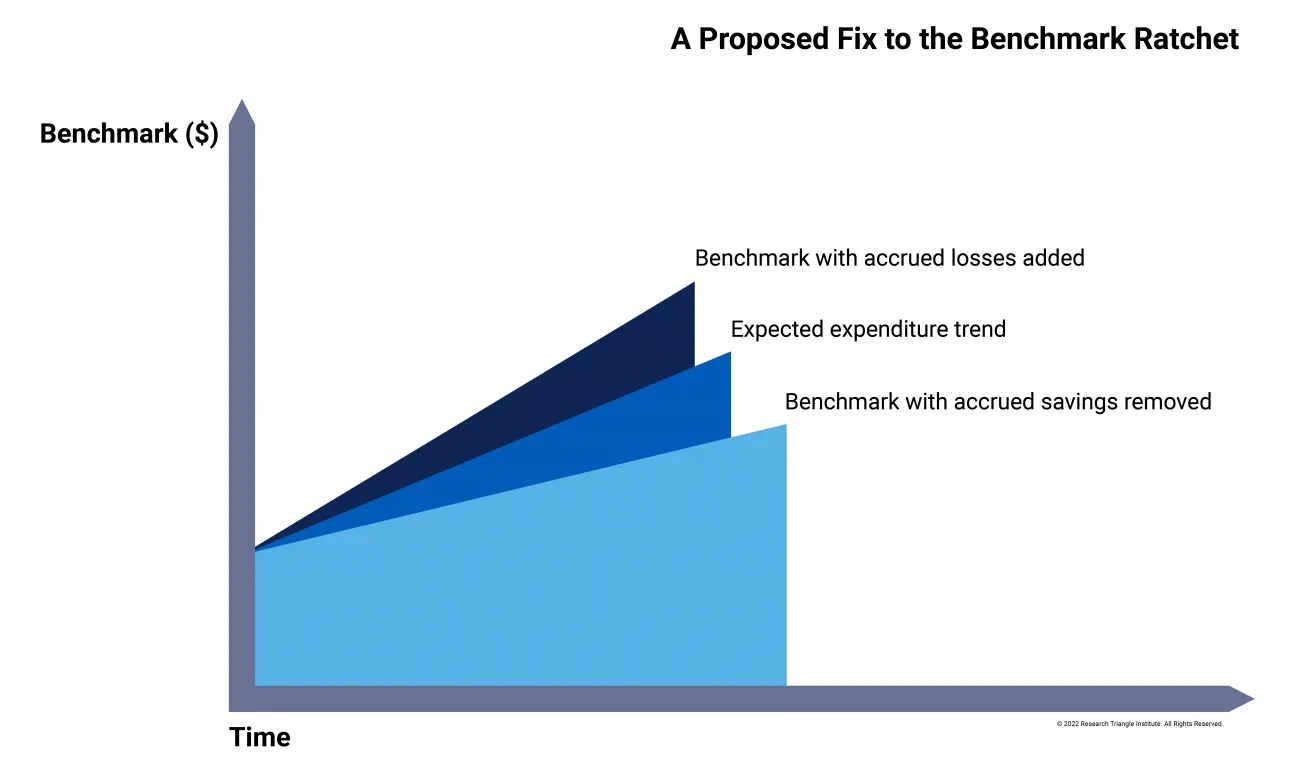
These “ratchet” effects reduce the incentive for successful ACOs—defined as those that reduce expenditures relative to the true, unobserved, counterfactual—to continue participating in future performance periods. Conversely, ACOs that increase spending are induced to continue participating because their elevated spending trickles into future benchmarks. A simple stylized example demonstrates this problem.
One way to fix the ACO benchmark ratchet
The method proposed by Brookings Schaeffer would redress these warped incentives by decoupling benchmarks from historic ACO expenditures. While initial benchmark levels would still be derived from historical expenditures, after a “convergence period,” benchmarks would be untethered to observed expenditures—internal to or external to the ACO. The authors assert that this would provide greater opportunities for providers to save and induce higher participation in ACO programs. The proposal contains the following components:
ACO benchmarks at the outset
At the beginning of an ACO’s participation in the APM, benchmarks for each ACO would be based on risk-adjusted historical spending. Incumbent ACOs would inherit previous benchmarks from existing methodologies subject to adjustments necessary to remove the accumulated ratcheting effect.
Convergence phase
During an initial convergence phase, benchmarks would be updated annually at the projected rate of Medicare fee-for-service (FFS) spending growth. The goal of the convergence phase would be to equalize benchmarks within a region gradually. Thus, ACOs with high expenditures for their region (who therefore inherit larger initial benchmarks) would experience slower benchmark growth during the convergence phase. Because ACO benchmarks would still be tied to historic ACO expenditures during this time, they would be annually adjusted for patient mix and provider composition.
Generating a “wedge” between ACO benchmarks and expenditure growth
To encourage ACO participation, benchmarks must grow faster than realized ACO expenditures. During the convergence period, benchmark growth rates would be smaller than projected FFS spending1 but exceed realized FFS spending. Over time, this would create a wedge between realized and projected FFS spending, increasing opportunities for ACOs to share in savings. Critically, because benchmarks would still be set lower than projected FFS spending, savings would still accrue to the larger system.
Section References
1. Projected FFS spending assumes the absence of ACOs or shared savings programs and accounts for both inflation and increases in volume and intensity of care
Regionally-based ACO benchmarks at steady state
Each ACO would receive the same baseline benchmark as others in their region following the convergence period. At the outset of this phase, the regional baseline benchmark would equal the weighted average of the most recent benchmarks of ACOs operating in the region. Each ACO’s final benchmark would simply be this baseline benchmark risk-adjusted for the patient mix.
ACO benchmark growth rates would be set administratively, entirely decoupled from growth in ACO expenditures, and vary regionally. They could be updated as needed to account for inflation, GDP growth, FFS spending trends, or unchecked growth in the gap between benchmarks and observed expenditures. In this steady state, an ACO’s spending at program launch would have no bearing on its benchmark and regional benchmark differences would result entirely from risk adjustment.
Advantages over current ACO benchmarking approach and other alternatives.
By decoupling growth in benchmarks from historic ACO spending, the proposed administrative benchmark approach removes the “ratchet” which squeezes ACOs beneath their prior savings. Other methods of dealing with this problem, such calculating benchmarks based on a wide regional area or removing an ACO’s own expenditures from regional expenditures, less directly correct the problem and introduce additional complications2.
This proposal also holds advantages over decoupling ACO benchmarks from historic expenditures by linking them exclusively to national FFS expenditure trends. This would require ACOs to outcompete one another to earn shared savings, which is suboptimal in a voluntary program where lowering systemic spending relies on inviting provider participation. Additionally, such approaches could result in under-provision of care as ACOs seek to stay beneath average FFS expenditures.
Relevance to commercial ACOs
Having been in existence since 2012, the Medicare Shared Savings Program experienced this benchmark “ratcheting” issue earlier than many commercial health plans. However, the core challenge remains the same for commercial payers who want to expand their ACO programs.
Tying ACO benchmarks to historic ACO expenditures, either directly through rebasing or indirectly through linking benchmark adjustments to regional expenditure trends, disincentives high-performing ACOs from participating. For commercial ACOs operating primarily in select markets, it may not make sense to link benchmarks to national trends. An administrative benchmarking approach like the one proposed here may be an attractive solution for encouraging provider participation while still incentivizing savings.
Work with the alternative payment model experts
Designing an ACO benchmark program is highly complex. Beyond the choices about benchmarking methodology explored here, payers need to decide how to phase in risk-based contracts, blend quality and cost incentives, approve provider lists for inclusion in ACOs, and attribute beneficiaries to ACOs.
RTI Health Advance’s experts in payment model design an evaluation have worked closely with CMS and commercial payers to design, implement, and analyze alternative payment models. As a consulting firm with the bones of a research organization, we are ideally suited to sift through the complex decisions involved in establishing a payment model and ensure that commercial models reduce cost, transform care delivery, and attract new providers.
Learn more about our payment and delivery solutions and our alternative payment model design and adoption services.
Section References
2. For instance, using regional trends to set benchmarks does not remove an ACO’s impact on its region. Removing an ACO’s expenditures from regional calculations introduces selection bias because patients not served by an ACO are a select, differentiated group. This issue is particularly large when an ACO has significant regional market share.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.