We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Rural Health Disparities: Changes And Challenges
The state of rural healthcare for people from racial, ethnic, or other underrepresented groups
What are health disparities?
Health disparities are differences in outcomes, health status, or disease burden among various groups of people.
What are health inequities?
Health inequities are social, economic, or environmental disadvantages that are systematic, avoidable, and unjust, often leading to health disparities.
Rural health disparities and the importance of quality measures
Rural communities face health disparities at higher rates than their urban or suburban counterparts. Quality measures provide standardized performance metrics that help healthcare leaders, policymakers, business people, and community advocates gain insights into where rural health disparities are improving, worsening, or creating a persistent challenge.
Persistent disparities challenge rural healthcare
Research shows that rural residents are more likely to be over age 65, experience poverty, have a poorer health status, and live with chronic health conditions.
| Rural | Urban | |
|---|---|---|
| Percentage of adults over age 65 | 17.5% | 13.8% |
| People living at poverty levels | 15.3% | 11.9% |
| Per capita income | $42,993 | $59,693 |
| Prevalence of adults with multiple chronic health conditions (e.g., arthritis, diabetes) | 34.8% | 26.1% |
Source: National Healthcare Quality and Disparities Report, Chartbook on Rural Healthcare, November 2021
The AHA’s Rural Report outlines the persistent, recent, and emerging challenges to rural healthcare:
Persistent challenges contributing to rural health disparities include longstanding realities of rural healthcare:
- Low patient volume makes it difficult to keep provider organizations open
- Heavy reliance on government payers equates to lower reimbursement to finance care
- Older populations with more chronic conditions make care more intensive and costly
Recent challenges are adding to the existing burden:
- Shifts from inpatient to outpatient care delivery exacerbate access and provider shortage issues
- Growing behavioral health needs where there are not enough professionals to meet the need
- Markedly higher costs for medication and insurance
Emergent challenges add further complexity to rural life and work:
- More frequent natural disasters, fires, drought, tornadoes
- Increased violence in the home and community
- Epidemics related to suicide and opioid-related deaths
Rural health disparities and mortality rate
Rural health disparities are growing as shown in the overall rural death rate. Between 1999 and 2019, the age-adjusted mortality rate for rural residents between 25 and 64 increased by 12.1%. This shift significantly widened the gap between rural and urban mortality rates. From 2017-to 2019, the average life expectancy in the U.S. was 77.5 years, with a 35.6-year gap between the lowest and highest life expectancy among all counties. The life expectancy expanse reflects the disparity in health between Americans who have better access to care, greater health literacy, and capabilities for advocating for self through healthy habits and preventive care.
COVID compounded these rural health disparities
COVID-19 has killed Americans living in rural communities at twice the rate of people living in urban areas. American Indian and Alaskan Native (AI/AN) people have the highest COVID-19 death rate at 281 per 100,000 individuals. Also, in rural counties where one BIPOC group comprises more than 33% of the population, death rates reach up to 2.1 times other groups. This could be due to rural vaccination rates being eight percentage points lower than urban areas (41% vs. 53%). Compounding the effects of the pandemic, 53% of rural residents have delayed or put off procedures and checkups compared to one-third of all Americans.
The effect of delayed care due to COVID-19 on population health is clear. For example, preventive cancer screenings dropped 90% or more for many health systems over the first four months of 2020. According to the National Cancer Institute (NCI), that drop in preventive cancer screenings could cause 10,000 preventable deaths over the next decade.
How are rural healthcare disparities improving, worsening, or becoming a persistent challenge?
The Agency for Healthcare Research and Quality (AHRQ) publishes the Chartbook on Rural Healthcare as part of their National Healthcare Quality and Disparities Report (NHQDR). It provides a comprehensive overview of the quality of healthcare received by the general U.S. population. It highlights disparities in care experienced by different racial, ethnic, and socioeconomic groups. Based on more than 250 measures of quality and disparities covering a broad array of healthcare services and settings, the last report was published based on data before the COVID-19 pandemic.
The following excerpted charts provide insights into where the U.S. is improving rural healthcare disparities and where there are persistent challenges or worsening trends.
Overall rural healthcare disparities quality measure trends
Access to care measures from 2000 through 2016-2018:
- 58% (11 of 20 metrics) improved
- 25% (5 of 20 metrics) stayed the same
- 20% (4 of 20 metrics) worsened
Racial and ethnic health disparities vary by group:
- 40% of care quality measures were poorer for Blacks and American Indians, and Alaska Natives than for Whites
- 1/3 of care quality measures were poorer for Hispanics, Asians, and Native Hawaiians/Pacific Islanders than for Whites
Healthcare disparities vary by residence location:
- 23.5% of care quality measures were poorer for residents of large central metropolitan areas than residents of large fringe metropolitan areas
- 33% of care quality measures were poorer for residents of *micropolitan and *noncore areas than residents of large fringe metropolitan areas
- <20% of care quality measures were poorer for residents of medium and small metropolitan areas than residents of large fringe metropolitan areas
*The Centers for Disease Control and Prevention (CDC) categorizes rural geographies as noncore or micropolitan.
Quality measures in rural communities that are worsening or remain low
The following charts are available via: National Healthcare Quality and Disparities Report Chartbook on Rural Healthcare. Rockville, MD: Agency for Healthcare Research and Quality; November 2021. AHRQ Pub. No. 22-0010.
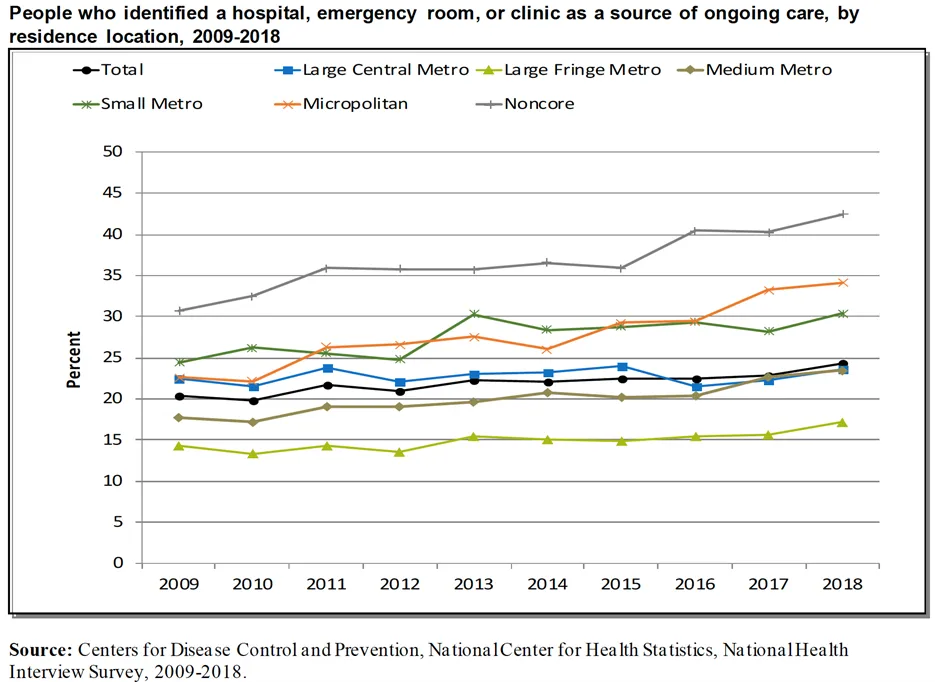
Using a hospital or emergency department as ongoing source of healthcare
In 2018, more than 40% of noncore and nearly 35% of micropolitan (both rural geographies) residents accessed ongoing care through a hospital or emergency room versus a primary or specialty care provider. This is significant because people who have a reliable primary care provider tend to have greater trust in the provider, good patient-provider communication, and a greater likelihood to receive appropriate care.
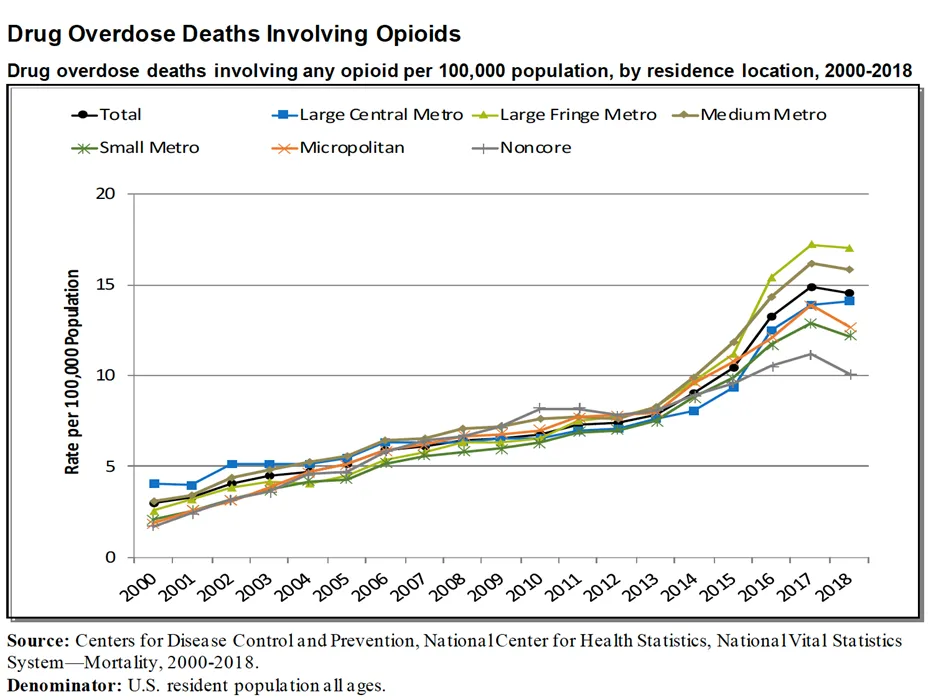
Drug overdose deaths involving opioid medications
A 2017 study on EHRs revealed that 14 of the 15 counties with the highest opioid prescribing rates were rural counties. Rural areas had higher rates of opioid-related deaths compared with urban areas. Between 2016 and 2019, age-adjusted drug overdose death rates in rural areas increased by 390%.
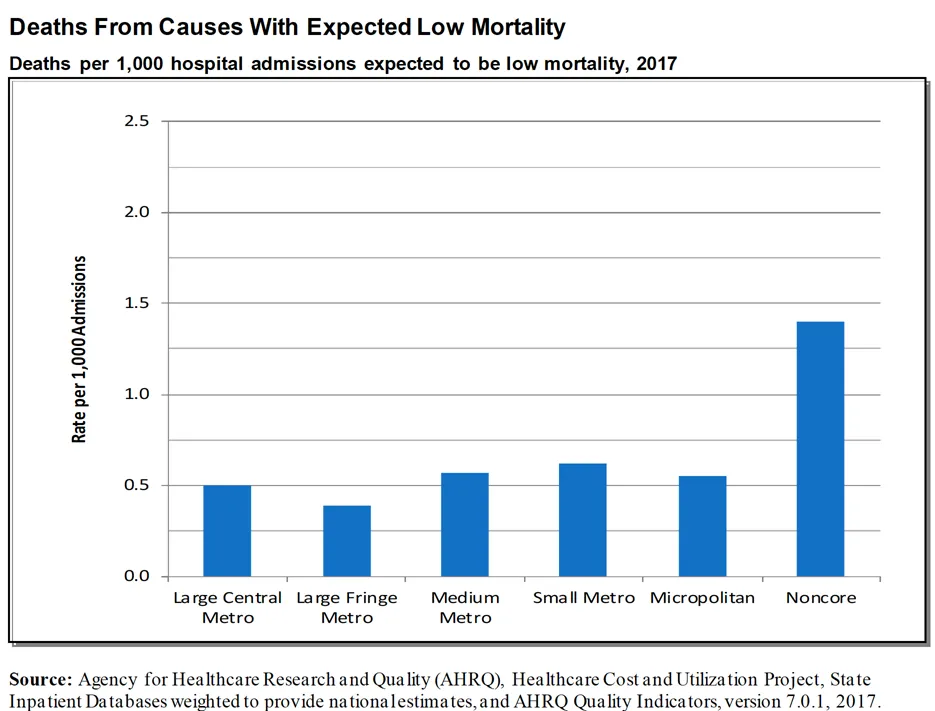
Premature death
Between 1999 and 2019, rural communities had the highest age-adjusted mortality rates compared with urban communities, increasing in absolute rates by 172%. Research has shown that rural counties that have a majority of Black or American Indian/Alaska Native residents have the highest rates of premature death compared with rural counties that are mostly White. Patients who were admitted to the hospital with low mortality had higher death rates.
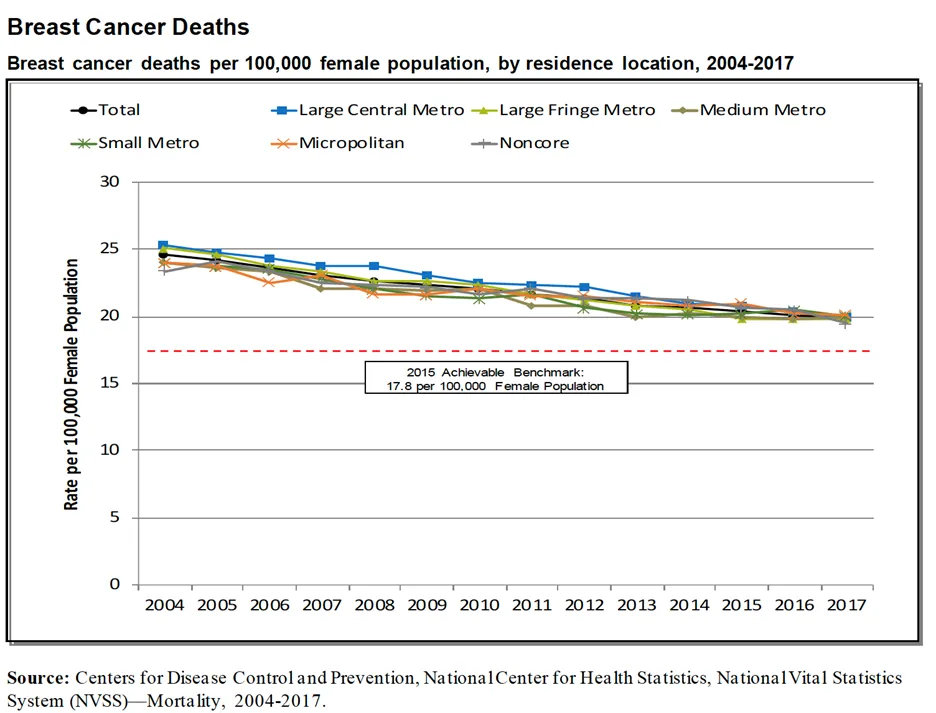
Breast cancer deaths
Between 2004 and 2017, deaths from a breast cancer diagnosis decreased across every geographic area, including rural areas. However, the decrease in death rates was not as significant for rural communities.
Creating positive change for rural health disparities
While rural health priorities have stayed consistent over the last decade, these data highlight where positive change is making a difference. However, persistent challenges remain and are significant. They are exacerbated by new disparities caused by COVID-19, increasing natural disasters, and changes in healthcare access.
Data analysis is key to prioritizing rural health equity initiatives
Learn more about RTI Health Advance services that can support rural healthcare initiatives, particularly related to Quality Improvement, Healthcare Data Analysis, and Health Equity Consulting.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.