We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Overcoming Mental Health Services Challenges In Rural America
Mental health has become a priority for individuals and communities. As healthcare professionals and stakeholders advocate for improved access to mental healthcare, rural areas emerge as a population experiencing substantial inequity.
Mental health disparities in rural America
Americans in rural communities have long faced an extensive list of health disparities, including those associated with chronic conditions like diabetes. Individuals living in places with populations fewer than 2,500 are more likely to die from disease and accidents than urban dwellers, namely:
- Cancer
- Heart disease
- Stroke
- Unintentional injury
- Chronic lower respiratory disease
- Motor vehicle crashes
- Opioid overdoses
In addition to these chronic health conditions, rural residents in the US also experience significant disparities in mental health outcomes—even though mental illness in urban and rural areas occurs at nearly the same rate. One of the most common mental disorders in the US is depression, which is slightly more prevalent in non-metro areas. Among individuals who received treatment, 58.4% of rural adults took prescription medication for depressive feelings compared to 48.6% of metropolitan adults.
Studies found that while rural adults were more likely to take prescription medication for depression, they were less likely to have seen a mental health professional and instead spoke with a general practice professional or primary care physician. Rural residents are also more likely to self-medicate in the following areas.
Alcohol
Roughly 1/3 of rural residents ages 12-20 abuse alcohol. Rural youth in this age group are more at-risk for underage drinking, binge drinking, cigarette smoking, tobacco use, methamphetamine, and opioids than their urban counterparts. The more rural the environment, the more likely it is that youth will consume alcohol or methamphetamines. They are also more likely to engage in high-risk activities like operating vehicles and machinery while under the influence.
Opioid Use
In recent years fatal opioid-related overdoses have surged in the US, topping 100,000 in 2021. Opioid-related hospital visits (ORV) between 2006-2013 increased at a higher rate than ORVs in urban areas. Among the states most affected by the opioid crisis are some of the most rural states by population: West Virginia, Ohio, and Kentucky.
Suicide
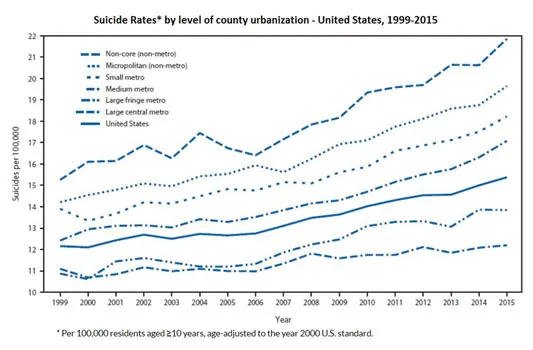
A CDC report found that deaths by suicide are significantly higher in rural counties than in urban counties and that gap is widening. Suicide in rural areas occurs at a rate of 18.3-20.5 per 100,000 residents compared to 10.9-12.5 per 100,000 residents in urban areas. Figure 1 shows the stark comparison. These numbers indicate that suicide is uniquely persistent and concerning among rural populations.
Additionally, native populations face disproportionally high suicide rates and mental health challenges in rural communities. Suicide numbers are likely underreported because, historically, data for indigenous communities have not been documented equally.
Why these disparities exist
While the need for affordable and accessible mental health resources is urgent among all populations, rural communities face a specific trio of challenges: accessibility, availability, and acceptability.
1. Accessibility
Accessibility in healthcare, according to the University of Missouri Center For Health Ethics, is "the ability to obtain healthcare services such as prevention, diagnosis, treatment, and management of diseases, illness, disorders, and other health-impacting conditions. For healthcare to be accessible it must be affordable and convenient."
Transportation
Travel is a significant barrier to accessing care. Residents of rural areas must often travel long distances to reach the closest mental healthcare facility. Often, this population experiences economic challenges related to transportation (finding affordable vehicles and paying for gas, insurance, and maintenance).
Public transportation to and from rural settings is limited. Non-profit organizations provide most public transportation options and the most common form of public transit is demand-response. In remote settings (less populated rural areas), travel challenges are compounded by seasonal weather patterns, which can block access to roads or make entering and exiting a facility hazardous.
2. Availability
For patients to access the mental healthcare they need, there must first be plenteous options and providers for them to choose from.
Provider shortages
One in 5 Americans live in rural America and 76% of all incorporated communities have populations below 5,000; yet mental health professionals are overwhelmingly centralized in metro areas. Ninety percent of all psychiatrists and psychologists and 80% of all clinical social workers practice in urban centers. The number of community mental health centers (CMHCs) in non-metro counties declined from 182 to 15 between 2000-2019.
In addition to provider availability barriers, there are financial limitations. Basic health programs (BHPs)—designed for low-income residents who are unable to purchase health benefits coverage through the Health Insurance Marketplace—typically operate in metro areas, leaving less affordable options in rural communities.
3. Acceptability
To advocate for mental health resources, society must be accepting of the need for these services.
Privacy and stigma
While stigma around mental health remains a challenge among all populations, unique factors influence stigma in rural communities. Ranchers, farmers, and other agricultural workers often internalize perceptions around strength and independence that can discourage them from seeking mental health support.
Residents of small towns where “everyone knows everyone," may have privacy concerns and fear that personal health challenges will become common knowledge in the community. In rural counties, a therapist or mental health provider could be a neighbor or local business owner, which can make seeking care uncomfortable. Patients may worry about someone recognizing their car in the mental health center parking lot or experience embarrassment requesting demand-response transportation if they know the driver or fellow passengers.
Health literacy in rural areas
Research suggests that individuals living in rural areas may have less overall health literacy, including mental health literacy. Without comprehensive knowledge, they may not recognize symptoms indicative of a behavioral health issue in themselves or others, and subsequently pass on opportunities to seek care.
Conversely, providers in rural areas may not recognize the root cause of a patient's symptoms since their patient population tends to focus on physical symptoms. Without early recognition or intervention, the behavioral health condition can worsen over time.
Cultural challenges to care
The shortage of mental health professionals is intensified by a lack of culturally competent care as rural areas become more diverse. In 2020, The Brookings Institution reported that 24% of rural Americans were people of color. The average rural county saw its population of color increase by 3.5% between 2010 and 2020, largely due to a substantial increase in the Hispanic population, which accounted for 52% of US population growth. More than half of American Indian and Alaska Native populations live in rural and small towns or tribal-designated areas.
Providers in these areas are typically not from the community in which they practice and may not look like many of the patients they treat. Language and communication barriers can make it difficult for providers to understand patient concerns, communicate treatment plans, and deliver care effectively. In more diverse rural areas, healthcare professionals may not have the training or experience to meet the intersectional needs of these populations.
Potential solutions
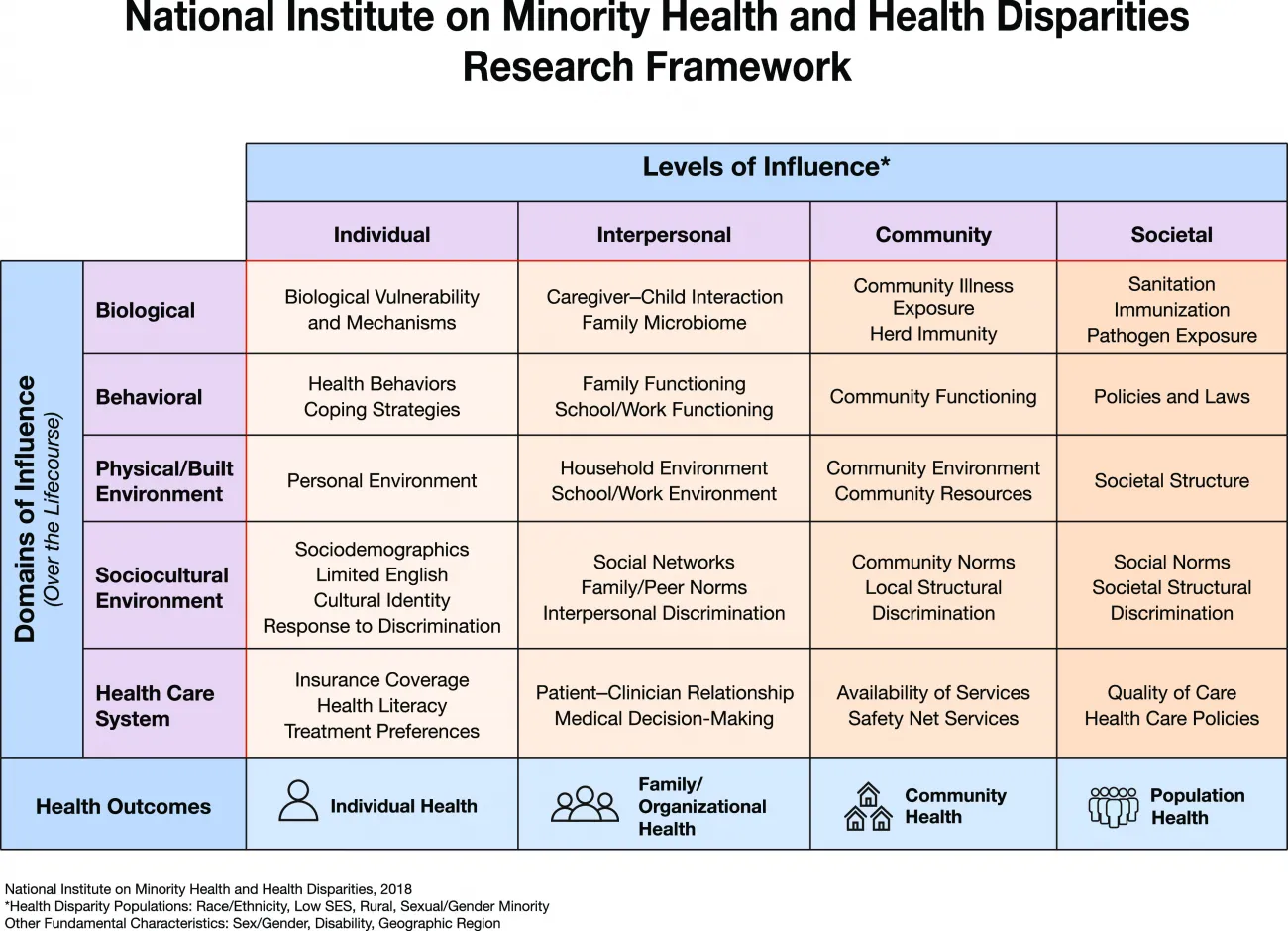
Rural mental health disparities derive from a wide-ranging list of complex factors that intersect many age groups, cultures, identities, and environments. The National Institute on Minority Health and Health Disparities (NIMHD) created a research framework that is especially helpful when applied to mental health. The chart in Figure 2 illustrates the multiple dimensions that affect mental health outcomes and is a useful tool when reviewing risk factors and ideating solutions.
Understanding the challenges that rural communities face is simply the beginning. Finding sustainable and effective solutions requires the collaboration of payers, providers, community-based organizations, and government agencies. Solutions that have worked in regions with more resources will require adaptation for the unique needs of rural communities or new ideas altogether.
Offer digital health tools
In recent years, telehealth has improved access to healthcare in urban and rural areas. However, digital health services still remain largely unavailable for residents of non-metro areas where cell towers are limited and many don't have internet access or a cell phone with a data plan.
Providers might consider allowing patients to use on-site facilities to access the internet for telehealth services. Engaging community members, such as libraries, schools, churches, and government facilities, can increase access to stable, high-speed internet.
Increase provider numbers
The correlation between rural counties and mental health professional shortages indicates that additional providers are needed to minimize disparities. Incentivizing providers to serve rural communities can help to increase the number of providers available. For example, there are few teaching hospitals in rural zip codes. Establishing paid internships or fellowships for providers to practice in rural areas is an option. Additionally, programs could offer incentives for student loan repayments if practitioners work in rural areas for a specified number of years after they complete a master's degree. Some states are currently considering programs that would allow providers with a bachelor's degree to treat patients who do not need serious long-term care.
Expand knowledge
These are several organizations working to expand mental health literacy in rural areas.
Mental Health First Aid hosts 8-hour workshops in over 27 countries that teach the following to participants in rural communities:
- Risk factors and warning signs for mental health issues
- Symptoms of depression, anxiety, trauma, psychosis, and substance use disorders
- A 5-step action plan to assess a situation, identify appropriate interventions, and help people access mental health services
- Available resources for individuals experiencing a mental health issue
Rural Minds is a nonprofit aimed at ending stigma around mental illness in rural America. They host webinars, source and dispense mental health information, and raise awareness through grassroots efforts.
Small Town American Media is a resource hub for rural communities. Their telemedicine efforts are aimed at helping Americans ages 65 and older—54% of whom live in rural towns—connect to healthcare providers.
Substance Abuse and Mental Health Services Administrations (SAMHSA), an arm of the U.S. Department of Health and Human Services, manages the National Suicide Prevention Lifeline and grants for suicide prevention, substance abuse, and mental health for specific populations, including rural communities, Native American populations, and veterans.
Create a patient advisory board
Start with community agencies and partners who are tuned in to residents' unique needs and ask current patients what services they need to feel welcome, safe, and confident as participants in their mental healthcare. Providers can also attend town hall meetings and school events: showing up physically and engaging with residents is one of the most powerful ways to promote trust within a community.
Train primary care staff to conduct mental health screenings
Assessing every patient for mental health risk factors can help identify potential illness so proper care recommendations can be made. Since most rural Americans receive the bulk of their care from primary care providers (PCPs), this is a natural way to integrate mental healthcare into the community.
Leverage alternative models of care
Collaborative care model - Under a collaborative care model, patients can have both their physical and mental healthcare needs met at the same location. Collaborative care relies heavily on screening. Once screened, patients are connected to an on-site behavioral/social/nurse healthcare manager for further assessment. This information is available in the electronic health system so providers can better identify who may need support right away.
Stepped care model - Not everyone is a candidate for long-term intensive therapy. Stepped care enables mental healthcare providers to practice at the highest level of their licenses. Therapists work only with the individuals who need it most while subclinical cases might be referred to a social worker or care manager. It's also critical under a stepped care model to offer multiple ways a patient can access care: in person, via telehealth, or a phone consultation line, for instance. Rural clinics and providers need flexible options, not a one-size-fits-all approach.
Create co-responder programs
Co-responder programs bring together behavioral health professionals and first responders, such as EMS and law enforcement, to respond to mental health crises. In states like Colorado and Montana, these programs have helped to de-escalate interactions between the community and first responders, increasing behavioral health support for individuals in crisis.
RTI Health Advance supports payers and providers delivering care in rural communities
Closing the gaps in rural mental health will require long-term change and investment. With the proper focus and dedicated effort, rural communities and their healthcare support systems can realize improved mental and physical health.
Our experts at RTI Health Advance support innovations for mental health in rural counties and lend trusted guidance on procedures and interventions designed to improve health equity. Contact us.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.