Case Study: Transforming Military Healthcare Through A Comprehensive, Whole Health Quality Framework
RTI Health Advance was engaged by a prominent military managed care contractor to support their transformation in providing healthcare to a large number of service members and their families. With a new contract to begin in 2024, this military health vendor wanted to evolve their traditional approach and services to prioritize performance outcomes, expanded services, interoperability, and beneficiary experience while realizing the Military Health System's (MHS) Quadruple Aim.
This case study reviews the challenges our client faced and its goals for the engagement. The approach taken by RTI Health Advance provided detailed recommendations the client could implement as part of a comprehensive, whole health framework. The framework, and its prioritized areas, are underpinned by a quality improvement model.
What does transformation look like for a modern military managed healthcare provider?
With payers leading the operational charge, the healthcare industry is transforming from Triple Aim to Quadruple Aim. This set of objectives centers on improved clinical outcomes, expanded access to services, and enhanced member and provider experience. The same is true for the Military Health System (MHS), one of America's largest healthcare systems and the world's preeminent military healthcare delivery system. The MHS works closely with the Defense Health Agency (DHA) and managed care contractors, such as our client, to execute the Quadruple Aim for military service beneficiaries and their covered family members.
The 2024 contract requires modernization modeled after civilian industry best practices
Our military managed care health plan client will begin a new contract in 2024 that seeks to modernize healthcare services modeled after civilian industry best practices. The client's transformation strives to realize the Quadruple Aim: improved readiness, better care, better health, and lower cost.
An evolution in the current clinical operating model and approach to quality is essential to successfully deliver on the expanded requirements outlined in the 2024 contract. The health plan's goal is bold: to be a clinical leader in shaping the development and implementation of a value-based care strategy, and the modernization of their services to align with the DHA. Critical to achieving their goal will include focus on 5 domains, including:
- Physical and behavioral health
- Patient experience
- Cost-appropriate care and effectiveness
- Care access
- Functional status and quality of life
Healthcare transformation includes clinical quality measurement and quality improvement
Additionally, the transformation process includes incorporating discrete performance measures that can be benchmarked, applied across all sub-populations, and tracked for year-over-year performance. Extending beyond standard HEDIS measures, our payer client aspires to meet the required expanded set of HEDIS measures prioritized by the DHA in the new contract that includes an incentive award for meeting challenging year-over-year quality benchmarks as a representation of the work being done to improve clinical quality outcomes. Lastly, addressing social determinants of health (SDoH) is a consideration as it influences all aspects of healthcare quality.
As part of the approach to clinical transformation outlined in the new contract, this client must identify and implement a plan to meet and sustain the initiatives and performance standards set by the DHA. The effort will advance a quality- and population-focused strategy, providing a solid foundation.
Successful execution toward this transformational vision, however, requires a sophisticated strategy and operating plan focused on members' increasing healthcare needs while striking a balance among organizational objectives, contractual requirements, and budgetary constraints.
Achieving these goals will set this military managed care company apart from the market, setting the bar high to provide beneficiaries with the quality, person-centric care they deserve.
Creating a framework for comprehensive whole health quality improvement
Transformation and modernization for this military managed care payer requires a tactical, phased approach based upon a comprehensive, whole-health set of quality domains reflective of the plan's covered population.
As a premier purchased care contractor and trusted DHA partner, our client partnered with RTI Health Advance to realize three outcomes, also identified in Figure 1:
- Identify quality strategy goals, outcomes, measures, and key populations.
- Evaluate the current quality, measure performance against future targets, and prioritize actions needed for success.
- Provide a portfolio of interventions and tactics informed by evidence and industry best practices to achieve quality outcomes, measures, and support identified vital populations.

Figure 1: Three target outcomes from partnership with RTI Health Advance.
The objectives of this project included developing an understanding of current clinical quality performance and operational initiatives and developing a best practice framework with priority recommendations that will impact population outcomes.
The consulting team evaluated performance data for 18 pre-identified, nationally-endorsed HEDIS quality indicators, completing an in-depth environmental scan of evidence-based and industry-leading interventions. These interventions offer a wide-ranging strategy for provider partnerships, value-based contracting, and beneficiary engagement to advance clinical outcomes and quality of care. RTI Health Advance prioritized the quality measures aligned with federal contract guidelines, pairing each with tailored strategies and interventions to drive performance improvement to promote overall military readiness.
In creating these recommendations, the RTI Health Advance team considered operational feasibility, industry best practices, workforce burden, current interventions, relevance to DHA priority areas, expanded requirements, and operational constraints. Ideally, transformation plans defined and prioritized specific clinical quality outcomes focused on initiatives that favorably impact business goals, DHA contract requirements, and the beneficiary experience.
Priorities and recommendations for military healthcare transformation
RTI Health Advance created a comprehensive framework after curating best practices, contract requirements, and assessing the client's clinical quality data. From that, the team crafted a list of impact initiatives based on industry best practices.
Creating a comprehensive healthcare transformational framework
The RTI Health Advance team used a mixed methods approach, including content onboarding sessions, key stakeholder interviews, an environmental scan, and a review of aggregate population data reports. A review of aggregate, market-level, and stratified population data was conducted to identify priority areas of need.
Then the team created a prioritization framework, shown in Figure 2, that focuses on achieving high-quality health outcomes, a medically ready military force, excellent patient experience with care, and fulfilled staff. The framework identifies priority clinical domains, recommended strategies, and outcomes that align with the client's objectives.
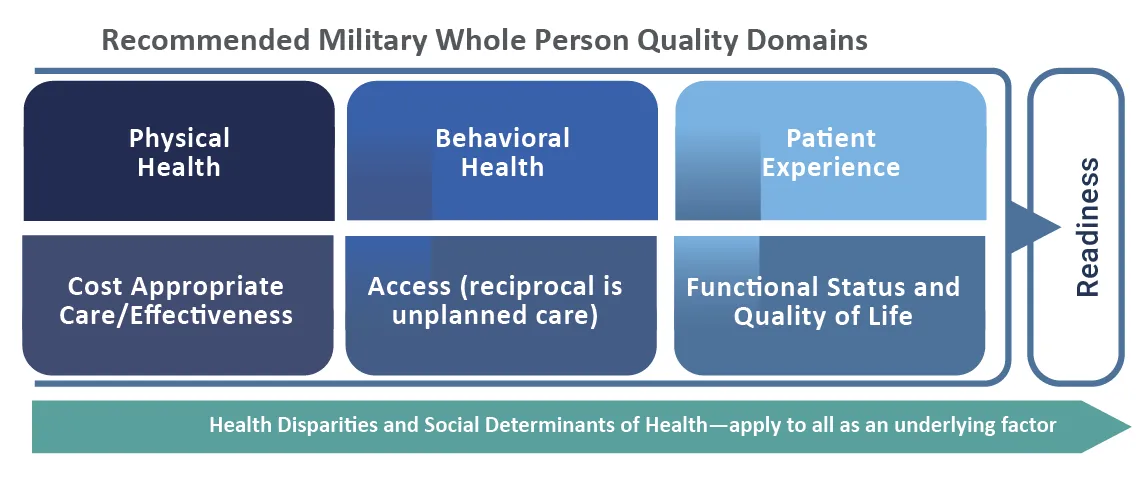
Figure 2: RTI Health Advance created a comprehensive framework that addressed quality and whole health priority recommendations.
Taking a “whole-health" approach to clinical quality domains
Although appearing national and population based in approach, many care models are limited in their ability to address a comprehensive, whole-health measurement of population health. Often, programs restrict their scope to claims-based administrative measures.
Our client had a unique opportunity to implement a vision based on a comprehensive set of clinical quality domains that, in total, will meaningfully impact outcomes of care for beneficiaries. Extending beyond HEDIS measures, RTI Health Advance's framework incorporates clinical quality domains that apply to all patients and populations regardless of sociodemographic characteristics such as age, gender, race, or ethnicity. Additionally, SDoH interventions were recommended as part of this client's vision of quality.
Recommendations for comprehensive clinical quality improvement
Figure 3 outlines the comprehensive set of clinical quality domains that RTI Health Advance recommended, which outlines 5 priority clinical domains, and provides targeted strategies, as well as specific targets for improved readiness and clinical outcomes. These domains are built upon a foundation focused on operational cultural change, enhanced data analytics, provider engagement, and beneficiary experience.
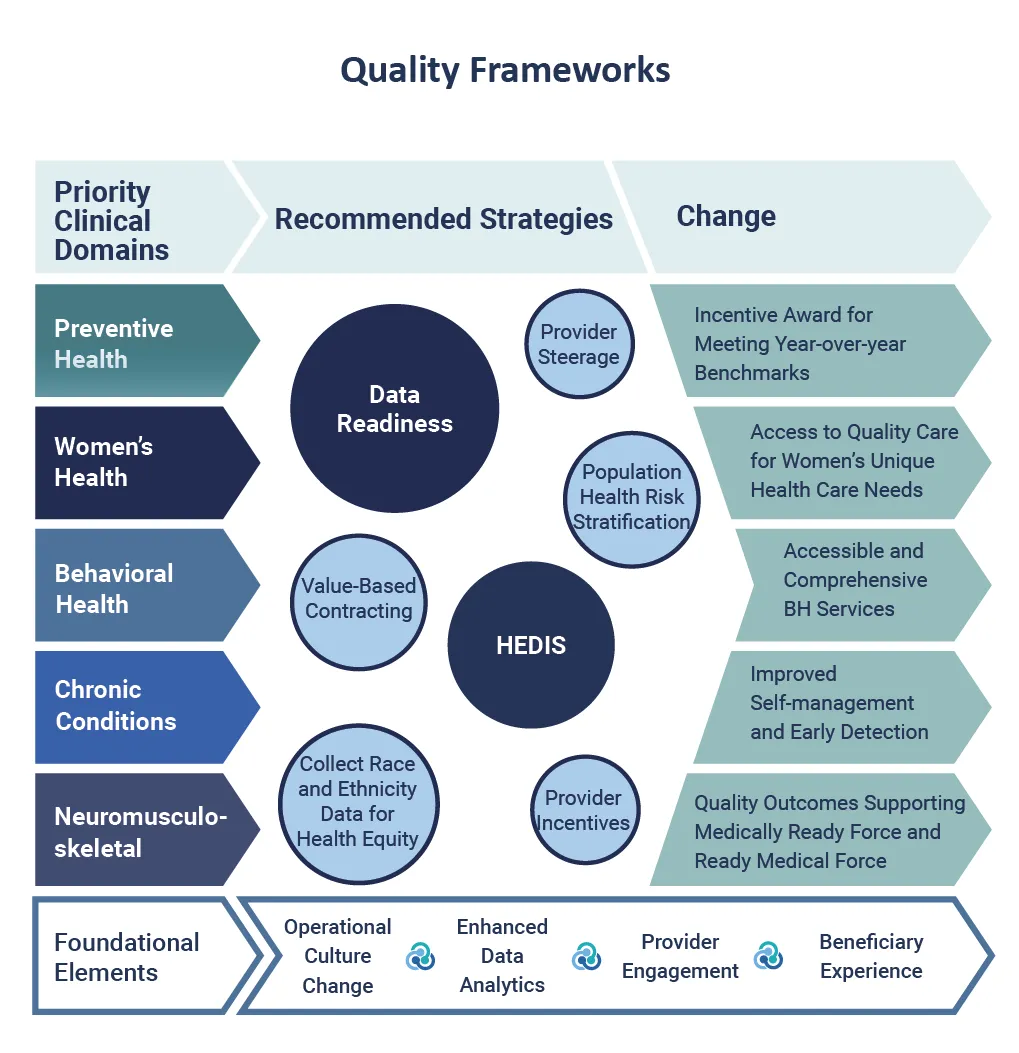
Figure 3: RTI Health Advance recommended a comprehensive set of clinical quality domains.
Clinical domain example: Preventive health
Of the 18 a contract incentive award fee measures, 10 are directly tied to preventive health outcomes. RTI Health Advance recommended several priority actions to achieve the performance thresholds. In particular, the team laid out an annual wellness campaign to close gaps in care within preventive health and support military family readiness goals. The program would specifically incentivize network providers in quality improvements efforts such as improved clinical documentation, clinical workflows, and data validation.
Foundational element example: Enhanced data analytics
One critical transformational objective is improving data readiness to ensure accurate, complete, and timely data. These are essential to tracking, analyzing, and improving quality outcomes. Sound data are important in quality improvement efforts, given that the data will be used to drive decision-making.
RTI Health Advance recommended standardizing how data should be reported and tracked and the goals for each quality-related metric. These efforts will help set the foundation for identifying opportunities for improvement. As opportunities are identified, the client can act on them by piloting interventions and evaluating their impact on quality outcomes and metrics.
As healthcare moves towards a more equitable future for all, the client's transformation toward value-based care is an ideal time to build health equity into the quality improvement framework as a priority area. Integrating health equity can be accomplished by collecting data on factors like race and ethnicity, and disaggregating data by patient demographics and geography to identify disparities in care, outcomes, and access.
Elevating health quality measurement beyond HEDIS
In addition to creating a comprehensive health quality framework specific to the client's beneficiary population, RTI Health Advance provided guidance on elevating their quality measurement beyond HEDIS to promote essential operations like those in provider-rating methodologies and value-based-care arrangements.
Building competency and capacity to transform healthcare
The consulting team also provided recommendations and actions to carry out their transformation, including:
- A priority list of clinical domains that could significantly impact the beneficiary population along with an array of population health, condition-management, and member-engagement actions to improve health outcomes for their military service members and families
- A blueprint, tailored to the population, outlining which quality measures and client service areas hold the highest opportunity for achieving quality measure benchmarks and impacting resource efficiency
- A set of prioritized operational strategies aligned with new contractual requirements and innovations for value-based payment models, addressing total cost of care, interoperability, local provider, and community partnerships
Special focus: clinical domains for quality improvement
RTI Health Advance provided this MCO client with key strategies across 5 priority clinical domains. Two included behavioral health and maternal and women's health with a cross-cutting focus on support for rural health.
Behavioral health
Prior to the current mental health crisis, the military population saw staggering impacts from behavioral health conditions: Veterans are almost twice as likely as civilians to commit suicide; between 2008 and 2017 more military service members committed suicide than died during the entire Vietnam War; and most individuals did not seek treatment prior to their suicides.
For this MCO, behavioral health is among the most prevalent conditions among beneficiaries, surpassing other highly prevalent physical health conditions such as diabetes, coronary artery disease, and asthma.
The RTI Health Advance team provided evidence-based recommendations to address access on multiple fronts, improve care navigation, expand virtual health, increase primary care integration, and provide a wider array of early intervention and self-directed education and support programs. Tapping into digital health and other in-home or on-demand resources was suggested as a way to further decrease social stigma.
Maternal and women's health
For this client, women's health is directly tied to military readiness. Individual Medical Readiness (IMR) can be more equitably achieved when a women's health programs and campaigns educate beneficiaries on preventive screening guidelines and connects them to available services. RTI Health Advanced recommended aligning programs with IMR and family health objectives by understanding areas of greatest need via stratification of women's health indicators beyond HEDIS metrics.
Suggested strategies to meet identified gaps and quality improvement goals include improving access to quality care by ensuring that network providers are available for preventive and emergent appointments across all market regions. Additionally, expanding the use of remote telehealth and telemedicine offerings can support expanded access.
Additionally, partnerships should be leveraged to maximize reach through community clinics and birthing centers, encouraging the use of certified doulas and midwives, providing maternal care education to mid-level and specialty practitioners.
Other foci were recommended to pursue specific improvements in hospital quality performance beyond preventative health. The shift to more purchased care off-base necessitates enhanced relationships with area hospitals to share data on beneficiaries and provide continuity of care that supports high-quality care.
Rural health
The RTI Health Advance team provided a host of targeted improvements and industry best practices that align with stated quality performance goals. Sample strategies included deploying mobile clinics to areas with identified need and engaging the Provider Contracting team to expand networks in rural areas. Digital and virtual health programs were fundamental to ensuring better access to beneficiaries in areas with limited access to providers such as those living in rural, remote, or deployment areas.
Empowering the client to transform healthcare for military service members and their families
Through a collaborative consulting engagement with this military managed care provider, RTI Health Advance provided specific insights, guidance, and strategy to execute their vision for the future benefits offered to military service members and their families, along with a detailed roadmap describing a multi-phased implementation of an advanced clinical operating model.
Now this client has the tools to realize a value-based future focused on tracking and improving quality-related outcomes, implementing quality improvement and will require refocusing mindsets, values, attitudes, and culture.
Healthcare quality improvement transformation starts here
RTI Health Advance works with healthcare organizations that are on a value-based care path and need to transform how they approach quality improvement, as well as track and assess performance measurement.
We meet each client where they are in their journey by evaluating the status quo, identifying a tailored menu of options that are appropriate and achievable, and work with them to implement evidence-based, best-practice approaches. Together, we can support clinical quality transformation in support of and emerging care and financial models. Contact us.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.