We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Section 1115 Waivers: Addressing Health-Related Social Needs
Section 1115 demonstration waivers provide states an avenue to test new approaches in Medicaid. Although the waiver program has been available since 1982, states are ramping up Section 1115 authority to address enrollees' health-related social needs (HRSN).
This overview article explains Section 1115 waivers and recent developments to promote coverage, access to and quality of care, improve health outcomes, reduce health disparities, and create long-term, more cost-effective alternatives or supplements to traditional medical services. We will also profile how waivers have been used to address social needs and provide insight into what states, payers, managed care organizations, and provider-partners can do to maximize their impact through these innovative payment and delivery models.
Current Section 1115 demonstration waivers focus on social needs
Both federal and state governments have identified addressing social determinants of health (SDoH) as a key Medicaid priority. Section 1115 demonstration waivers offer a clear path to design, research, and pilot new programs or reimagine existing ones.
States are encouraged to propose waivers to achieve 4 objectives:
- Expand Medicaid coverage
- Reduce health disparities
- Advance whole-person care
- Address health-related social needs
Current and pending waivers encompass a wide range of programmatic goals, including comprehensive changes in Medicaid eligibility, benefits, and provider payments to:
- Expand specific eligibility criteria
- Enhance benefits like those for behavioral health
- Implement SDoH provisions for social need
- Address needs of particular populations or benefits
Figure 1 shows where approved and pending Section 1115 waivers focus with 67 approved waivers in 48 states and 32 pending (as of February 2, 2023) in 28 states. Most are oriented toward expanding eligibility and particular benefits, while the third largest is for SDoH and social needs.
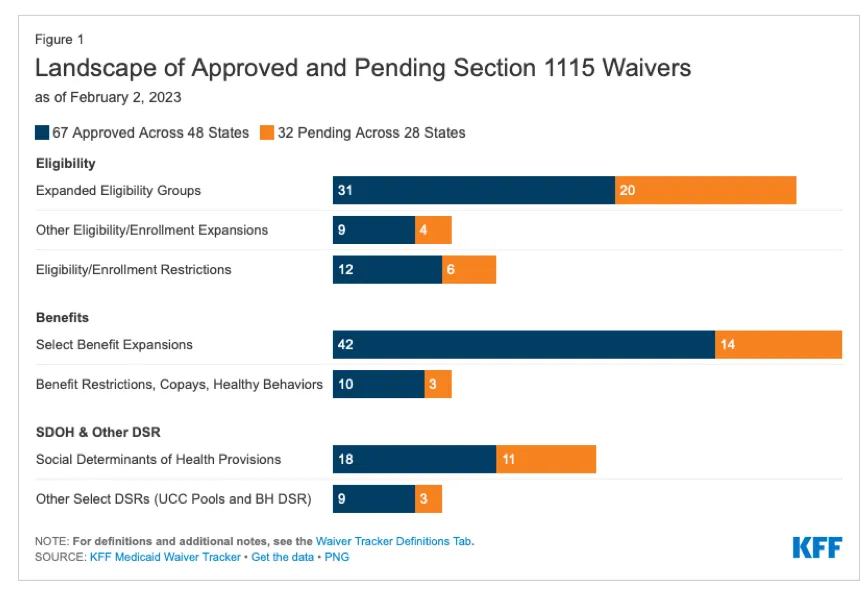
Figure 1: Landscape of Approved and Pending Section 1115 Waivers. Source: KFF Medicaid Waiver Tracker
Which states are pursuing social needs Section 1115 waivers?
While encompassing a small share of the overall Medicaid population and Medicaid spending, health-related social needs inclusion is expected to create positive change. According to CMS, it will “promote coverage, access to and quality of care, improve health outcomes, reduce health disparities, and create long-term, more cost-effective alternatives or supplements to traditional medical services."
Among all the pending and approved waivers, 4 states (AR, AZ, MA, and OR) have included health-related social needs services for specific groups of enrollees. KFF's Section 1115 Waiver Tracker (labeled as Table 1) provides a snapshot of the types of health-related social needs provided to defined populations for housing, nutrition, and other supports like case management and transportation.
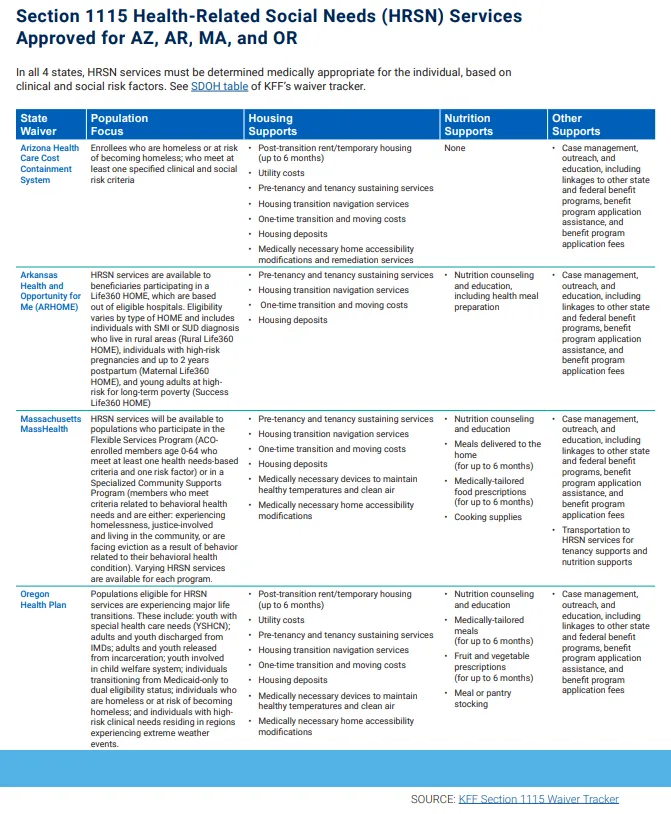
Table 1: KFF Section 1115 Waiver Tracker. Click here for PDF.
How states are using waivers to address social needs
Three snapshots demonstrate where states' waivers overlap or are working to address common issues and how they can tailor benefits to meet their regional and specific population needs.
California: CalAIM (California Advancing and Innovating Medi-Cal) is a 5-year program (2022-2027) that builds on the success and learnings of a previous 1115 waiver when they created a whole-person care approach and the Drug Medi-Cal Organized Delivery System. Expanding statewide while integrating more seamlessly with social services, managed care plans can provide any of 14 support services, including:
- Post-hospitalization housing
- Enhanced care management
- Caregiver respite
- Food and nutrition support
- Transition assistance from nursing home care
North Carolina: Launched in Spring 2022, the Healthy Opportunities Pilots (HOP) focus on housing instability, transportation needs, interpersonal violence, and chronic stress for high-need managed care enrollees with specific health and social risk factors. As a 5-year waiver program, HOP covers the cost of 29 interventions chosen based on their potential to improve health outcomes and lower healthcare costs. Case managers at 5 health plans covering most Medicaid beneficiaries act as the program's gatekeepers. As of January 2023, over 3,000 enrollees had received over 27,000 services. HOP's website highlights some of the health-related social needs assistance offered:
- Funds for utility payments
- Income-based housing voucher transfers
- Healthy food boxes
- Funds for automotive repairs
- Funds for Winter home repairs and maintenance
Washington: The Taking Action for Healthier Communities (TAHC) program is a renewal and extension of their original waiver for the Medicaid Transformation Project (MTP). MTP 2.0 taps into their Accountable Communities for Health, creating 10 community hubs as part of investments into multi-sector, community-based partnerships and approaches. This waiver's 4-year goal is to connect social and public health with community-based organizations to create a clinical-social delivery system. The program focuses on 3 overarching goals:
- Expand coverage and access through an Apple Health program
- Advance whole-person primary, preventive, and home- and community-based care with integrated behavioral health assessments
- Accelerate care delivery and payment innovation focused on health-related social needs
Examples of health-related social needs benefits include:
- Extending postpartum service coverage
- Re-entry coverage for formerly incarcerated individuals
- Expanding substance use disorder and mental health benefits
- Long-term services and supports
- Implementing a standardized and integrated physical-mental assessment
Engaging a QI approach for successful social need Medicaid 1115 waiver pilots and programs
Many health-related social needs waivers are extensions of previous programs, while others bring an SDoH focus to Medicaid programs for the first time. Implementing, managing, and supporting a successful Medicaid 1115 waiver program requires a quality improvement (QI) approach across 3 areas. An iterative QI model enables program leadership to use required cycle evaluations as an opportunity to report, learn, and improve.
1. Waiver program strategy, implementation, and operations
The Section 1115 demonstration waiver application lays out the objectives of the program and the specific program elements, policies, and strategies that will be used to achieve desired improvements in health outcomes, quality of care, and Medicaid cost impact. Translating the application into a program that can be implanted takes another set of skills and experience. Pilot programs tend to struggle with several capabilities, including:
- Attracting qualified program candidates
- Enrollment and onboarding
- Creating adequate referrals for health-related social needs services
- Communication within the program and among community and social support organizations
- Coordinating data, documents, and activities using technology
- Education inside and outside the program to ensure all program staff can manage their part of the referral workflow
- Referral follow-through to ensure needs were fulfilled
- Operation administration for funding and invoicing from community-based organizations and payments through network hubs
2. Promotion and program outreach
One of the challenging parts of ramping up a new program is identifying the most appropriate candidates, engaging them, and ensuring they can access the information and services needed. A community outreach plan is crucial and should include stakeholders from program leaders to educators to frontline staff who consult with participants. Communication and education via promotion and program outreach ensure that the identified population knows about the program, how to enroll, and how to maximize their participation.
3. Monitoring, evaluation, and reporting
Medicaid requires evaluation of health-related social needs initiatives to guide current funding and priorities for each program and inform future policy decisions about whether and how to use Medicaid funding to address enrollees' social needs.
Section 1115 waivers are subject to monitoring and evaluation requirements that increased under the ACA. States must make their CMS-approved evaluation strategy publicly available. The strategy must include measurement criteria related to coverage, access, and outcomes. For example, states must regularly collect and report data that will answer questions about the number of enrollees served by the health-related social needs initiatives, including:
- Prevalence and severity of the enrollees' social needs
- Enrollee utilization of preventive and routine care
- Utilization of potentially avoidable, high-acuity care
- Cost effectiveness of health-related social needs initiatives
- Impact on overall access, quality, and health outcomes
- Positive changes in health disparities
Evaluation requirements also include a schedule of deliverables with quarterly and annual monitoring reports, interim and final evaluation reports, and a summative evaluation.
Health-related social needs waivers could advance social risk interventions and managed care organization programs
According to a February 2023 article in JAMA, “these new waivers represent a noteworthy departure in approach, treating specified health-related social needs services as a Medicaid benefit."
The federal government's pending rate for covering health-related social needs benefits could be substantially higher than the rate for health-related services. Creating a health-related social needs benefit could significantly advance investments in social risk interventions for Medicaid beneficiaries. Over the next 5 years, this wave of waiver programs could determine how well managed care plans can address social factors that affect health.
RTI Health Advance supports states, managed care organizations, community-based organizations, and waiver program partners
Our multi-disciplinary team spans all areas needed to submit and implement a successful Section 1115 demonstration waiver, including areas like health equity, population health, payment reform, digital health, and quality improvement. Whether you've already submitted or been approved, we can help you create or expand effective health-related social needs benefits and SDoH interventions. Contact us.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.