We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
Medicaid Health Equity Requirements: What States Are Incorporating & Incentivizing
States are adopting health equity quality measurements as part of CMS's and Medicaid's commitment to identify and address health inequities. Part 1 of this series examined how states are integrating health equity measures and requirements into Medicaid programs. It took a close look at NCQA's Health Equity Measurement Framework, which offers a set of 21 measures curated from existing frameworks.
In Part 2 of this article series, we're now examining how states are incorporating, incentivizing, and requiring the adoption of health equity performance measurements and other health equity improvement activities. States' success stories demonstrate how innovative approaches create positive change and how survey results indicate states' near-term plans.
Health equity measures and new requirements part of Medicaid program improvements
In recent years, the federal government and many states have moved beyond identifying health equity as a key Medicaid priority to make material progress toward a foundation that supports health equity improvements.
According to MACPAC's 2022 Report to Congress on Medicaid and CHIP, "At the federal level, HHS and CMS have made commitments to these efforts, but specific action steps are still under development. State Medicaid programs have also shared their intentions and initial steps to promote health equity, and many are examining their programs and policies…"
These health equity improvement efforts include:
- Improving Medicaid race, ethnicity, and language (REL) data collection and stratification
- Tying financial incentives to health equity-related performance goals for fee-for-service (FFS) and managed care organizations (MCOs)
- Requiring health equity assessments and the creation of health equity strategies and plans
- Requiring performance improvement projects (PIPs) focused on health disparities
- Requiring various health equity efforts like training, job roles, progress reporting
Because Medicaid is a state-run program, state Medicaid offices choose, implement, and govern any requirements, including those that are related to health equity. As we'll see, these requirements and plans vary considerably by state.
States' health equity requirements focus mainly on MCOs through VBC payment models
Published by Kaiser Family Foundation (KFF), Healthcare Management Administrators (HMA), and the National Association of Medicaid Directors (NAMD) in October 2022, results from the Annual Medicaid Budget Survey for State Fiscal Years 2022 and 2023 outline the percentage of states that have made concerted efforts related to health equity:
- 66% of states are using strategies to improve REL data
- ~ 25% of states are tying MCO financial incentives to health equity
- Some states are beginning to leverage MCO contract requirements to promote health equity
It's important to note that most states pursuing health equity requirements, including financial incentives, are in Medicaid managed care arrangements like MCO, Primary Care Case Management (PCCM), prepaid health plans (PHPs), or others.
KFF's Medicaid annual report and survey revealed, for example, that only 2 states reported FFS financial incentives in FY 2022. Another 5 plan to launch new incentives in FY 2023. And, because capitated managed care is still the predominant delivery system for Medicaid in most states, this piece will mainly focus on MCO requirements.
MCO health equity requirements and recommendations
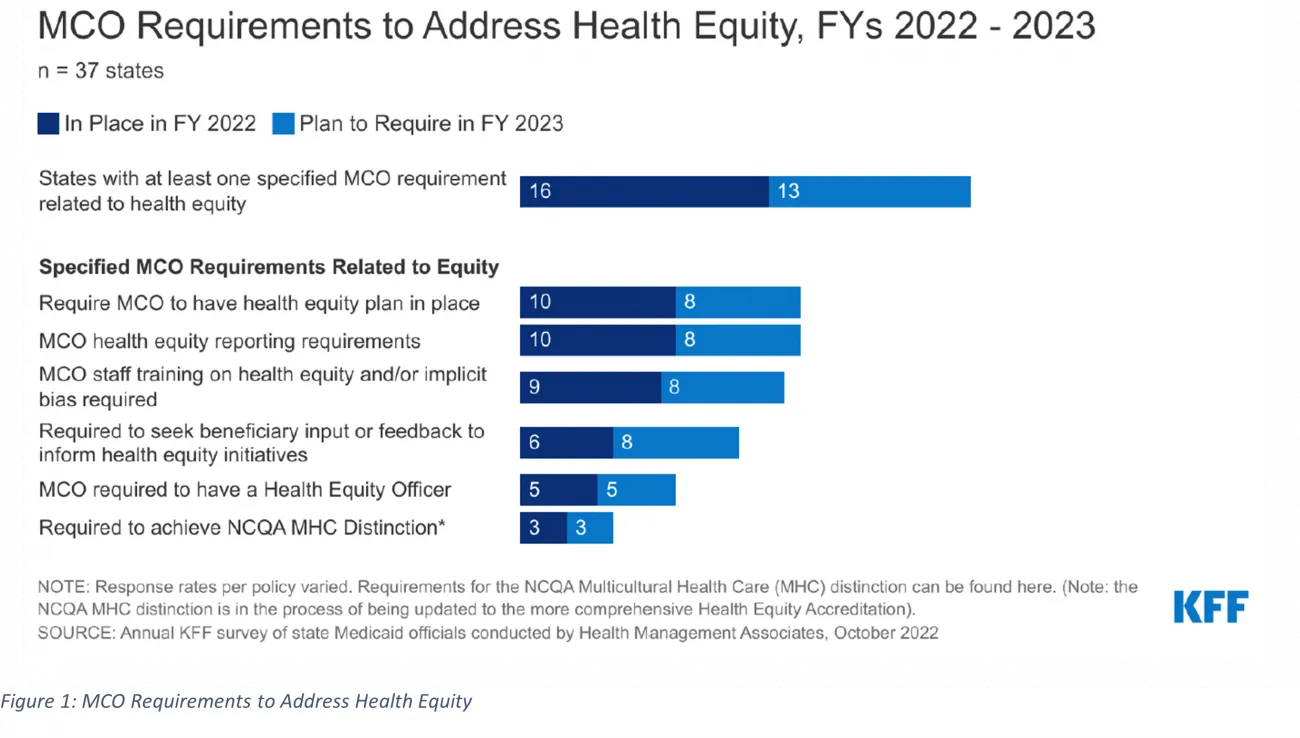
Currently, there are few health equity-related requirements; most are recommendations. Related to health equity measures, there are several that states have adopted or plan to adopt in the near term. States are establishing a variety of requirements for MCOs, including:
- Achieving national standards for culturally competent care
- Conducting health equity training and/or education on implicit bias
- Requiring particular roles like a health equity officer
- Reporting racial disparities data
- Incorporating enrollee feedback
Figure 1 illustrates which health equity-related requirements are trending in FY 2022 and FY 2023. The data from KFF also show that states with these requirements will stay the same or double in FY 2023.
For example, 50% of responding MCO states (16 of 37) had at least 1 health equity MCO requirement in FY 2022. That number is expected to grow significantly in FY 2023 (from 16 to 25). Other states with no equity-related requirements for MCOs planned for this year are considering or planning to adopt them. If this trend continues, half of all states will have some health equity-related requirement in FY 2023, extending Medicaid's commitment to addressing health inequities.
Medicaid Core Set as a health equity requirement
According to the policy think tank AcademyHealth, 15 states "currently require their MCOs to report health equity-related measures with additional measures and Medicaid programs to come."
The Medicaid Core Set is the most prevalent set of measures that states may require. For adults, the measures align with CMS's health equity priority areas, focusing on primary and preventive care, maternal and perinatal health, care of acute and chronic conditions, behavioral healthcare, and patients' experience of care. Together, the Child and Adult Core Sets provide a standardized, nationwide measurement tool for monitoring and improving the quality of care paid for by Medicaid.
While reporting the Medicaid Core Set for adults and children is voluntary, numerous states are evaluating their programs through a health equity lens by requiring Medicaid Core Set quality of care performance measures. These data are typically collected from health plans as part of quality evaluation and should be stratified by race or ethnicity. The core's overlap with HEDIS measures aims to make reporting easier.
Michigan, for example, requires MCOs to report select Medicaid Core Set measures stratified by race and ethnicity. Those MCOs must include these measures in their annual health equity report. The state analyzes these measures to set goals, including health equity priorities.
Additional Core Set requirements coming for FY 2024
Beginning in FY 2024, all states will be required to report on the core quality measures for children enrolled in Medicaid and CHIP. Additionally, the core behavioral health measures for adults enrolled in Medicaid will be required.
As part of the Workgroup for the 2023 Child and Adult Core Set Annual Review published by Mathematica, health equity was a "special topic." The workgroup's desire is "to address social determinants of health in the Core Sets" along with aligning "efforts across federal agencies to develop, test, and adopt standardized quality measures for state-level reporting."
NCQA Distinction in Multicultural Health Care designation
The NCQA Multicultural Health Care Distinction (MHCD) evaluates and recognizes health plans and other organizations for meeting rigorous standards in serving people with different racial, ethnic, linguistic, and cultural backgrounds. To date, 84 organizations are recognized with Distinction.
The program also aligns with NCQA Health Plan Accreditation/Plus and demonstrates performance in 5 areas:
- REL data collection and analysis
- Language services
- Practitioner network cultural responsiveness
- CLAS standards program, providing culturally and linguistically appropriate services
- Reducing healthcare disparities through targeted interventions, analysis, and patient experience
Pennsylvania Medicaid, for example, requires its managed care plans focused on physical health to earn MHCD. This requirement was chosen after researchers determined that some of Pennsylvania's MCO plans have substantially lower primary care access and emergency department utilization disparities. MCO plans, as a result of this requirement, report care quality improvements for those plans who have achieved MHCD.
Of the 84 organizations that have achieved the MHCD designation, 80 have received, or are in the process of receiving, NCQA Health Equity Accreditation or Health Equity Accreditation Plus. Six have completed all 3 designations, indicating growing adoption for MHCD and commitment to health equity through accreditation.
Financial incentives and payment models encourage and reward health equity efforts and performance
Tying financial incentives to health equity-related performance goals is the most significant lever states use with FFS plans and MCOs. According to KFF's survey, nearly 25% of responding states (12 of 44) had at least 1 financial incentive tied to health equity in FY 2022. Five additional states are planning incentives for FY 2023. Most incentives tied to health equity performance are set for MCOs, with only 2 states using incentives for FFS.
These inducements could include performance bonuses or penalties, capitation withholds, or value-based state-directed payments to quality measures. With MCOs, states most commonly utilize capitation withholds, pay-for-performance incentives, and state-directed provider payments to health equity-related quality measures.
Examples of how states have creatively used financial incentives for health equity performance
Connecticut established an obstetrics pay-for-performance program 6 years ago, focusing on at-risk pregnancies. In FY 2023, the state is launching a maternity payment bundle, tying financial incentives to health equity outcomes. Benefits will expand to include doulas and breastfeeding support.
In FY 2022 and FY 2023, Michigan will use part of its MCO capitation to withhold pay for performance payments based on health equity-related HEDIS measure performance and shared metrics that address health equity through coordination with behavioral health prepaid inpatient health plans (PIHPs).
Similarly, Louisiana indicates in its MCO re-procurement process that it may withhold 2% of the monthly capitation payment to encourage quality, health outcomes, value-based payments, and health equity. MCOs can earn back the withhold based on their health equity requirements reporting and performance.
During the pandemic, Ohio, Oregon, and Wisconsin implemented MCO incentives related to COVID-19 vaccination rates.
These examples show how states are integrating health equity performance requirements. Through requirements and financial rewards, these states establish measurable priorities and denote requirements toward closing disparity gaps and improving health equity for all Medicaid and CHIP enrollees.
Federal Medicaid requirements for performance improvement projects
Federal requirements also support health equity measurement and performance through Medicaid managed care regulations. States must ensure that their MCOs develop and publicly post quality strategies that include plans to reduce healthcare disparities. MCOs and PHPs are required to establish and implement a comprehensive quality assessment and performance improvement (QAPI) program for Medicaid services that includes Performance Improvement Projects (PIPs). For FY 2022, nearly 50% of states surveyed (17 of 37) indicated that they require MCOs to participate in PIPs focused on health inequities.
Examples of health equity-related PIPs implemented by states include:
- Maternal and child health
- Social determinants of health assessment, referral, and follow-up
- Diabetes education and management
- Substance use disorders
- Access to culturally and linguistically appropriate services
Three states require all PIPs include a health equity component or equity and disparities analysis. Other states require MCOs to engage in at least 1 PIP focused on health disparities, and 1 state requires MCOs to collaborate with other MCOs along with the state on a statewide PIP addressing health equity.
Because PIPs are federally-mandated, states have leverage to integrate health equity requirements that can be fulfilled through performance improvement efforts.
State Medicaid has support to embrace health equity performance further and establish impactful requirements
State Medicaid is at the forefront of efforts to care for people who may struggle most with health disparities. Their managed care and risk-based arrangements, along with support programs and requirements to innovate around health equity, give states the power to cause positive change.
As states establish and test health equity measurements and requirements, they will encounter issues where they may need outside support, technology, and expertise. These areas could include:
- REL data capture, accuracy, and analysis
- Health equity framework selection and implementation
- Health equity measurement reporting management and analysis
- Quality improvement oversight to ensure outcomes are used to improve access and care while addressing health disparities
There are a number of priorities for states: preparing for the unwinding of the COVID-19 public health emergency while also prioritizing health equity. External support in 1 or both areas can help states adopt health equity quality measures in keeping with CMS and Medicaid requirements.
RTI Health Advance offers a team of experts across the spectrum of managed and value-based care. From health equity, data analytics, quality improvement, population health, and digital health technologies, we can help you achieve care, quality, and cost goals that account for the unique needs of a state's Medicaid enrollee population. Contact us.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.