We've joined our RTI Health Solutions colleagues under the RTI Health Solutions brand to offer an expanded set of research and consulting services.
How Are States Integrating Health Equity Data and Measures Into Medicaid Programs?
Medicaid covers 20% of Americans and 60% of those covered are from historically marginalized races or ethnicities. This makes it critical that state-based programs embrace health equity and requires more of their contracted health plans and managed care organizations (MCOs). Medicaid influences many categories of payers, types of provider organizations, and how value-based arrangements prioritizes which healthcare services.
In Part 1 of this article series, we'll explore this topic from the vantage point of the NCQA's Health Equity Measurement Framework. In Part 2, we'll examine how states are incorporating and requiring the adoption of health equity measurement and performance reporting.
Stratified health disparity data and reporting are crucial, yet lagging
Data and performance measures are two critical aspects of addressing health disparities. They not only create the input to programs and interventions, but they also form the output that demonstrates progress and improvement. The collection of data and reporting on health disparities has progressed slowly, though, since the ACA was signed into law in 2010.
The National Health Law Program published a position piece in 2021 pointing to key Medicaid legislation and requirements that have fallen short related to health equity. In 2016, new requirements asked states to describe a plan to decrease health disparities in their quality strategies. Even with this requirement, as the author notes, “little has happened." It seems that until recently, health equity efforts by Medicaid have fallen short.
For example, AHRQ has published quality and outcome trend reports since 2003. The most recent is from 2021 and highlights a number of improvements, though health equity is only mentioned twice in the report.
Highlights from the AHRQ 2021 quality and outcomes trend report:
- A 24% reduction in the number of measures used in CMS quality programs.
- Increased focus on outcomes measures, which increased from 39% to 46% of total measures since 2015.
- Transition to digital measures, accounting for nearly 80% of measures in 2020.
- Significant costs avoided calculated for a small subset of 15 Key Indicator measures, yielding total estimates ranging from $29.6 billion to $51.9 billion.
- 34% of Key Indicator measures analyzed with baseline disparities showing improvement in at least one measure performance comparison.
These improvements show the importance of outcomes measures and the potential for pursuing health equity measures and reporting.
Health disparities show mixed results for Medicaid beneficiaries
Related to improvements in health disparities for Medicaid beneficiaries, the report shared both declining and positive movement:
Improving measures: Among 59 key indicator measures with a disparity in the first year, 34% showed improvement in at least one measure performance comparison. Disparities between subgroups and reference groups improved in comparisons based on income (9 of 34), dual eligibility (4 of 18), urban/rural location (8 of 20), and race/ethnicity (24 of 120).
Declining performance: Nine percent of all measures analyzed and five percent of Key Indicator measures had declining performance from 2013 to 2018, as reported in 2021. This percentage represents persistent disparities in 154 measures and 46 new disparities across race/ethnicity, location, and income.
Results like these highlight the need to pursue health equity initiatives for Medicaid recipients and further ramp-up structured plans, measures, and performance reporting.
Health equity plans are just the beginning
A few states have communicated health equity plans — like Colorado in 2019, Delaware in 2018, Nebraska in 2020. Some plans mention health equity, but don't specify plans for reducing health disparities.
Until now there have been significant gaps in core measures and, where there are core measure sets, few states stratify for race, ethnicity, disability, or other demographics. Minnesota and Michigan are two states who do stratify to some depth.
Recent changes strive to increase accountability for reducing health disparities
The first change requires all states begin reporting on two measure sets-behavioral health and childcare-by 2024. The second change was NCQA's proposal in February 2021 that requires payers to report measures with stratification within three years. They recommended stratifying five measures in 2022 and 15 in 2024. A third development is that CMS establish value-based payment models with equity requirements that will affect states as well.
When viewed with a historical lens, these changes are important shifts and new requirements to increase transparency and accountability. These promising changes may reveal insights that can improve care, outcomes, performance, and financial rewards.
The NCQA is taking an important lead for state Medicaid programs and their contracted health plans
As the major health plan accreditor and the steward for the most widespread national quality measure set, the NCQA has gone further by creating a new measurement framework for Medicaid that centralizes health equity within quality measurement.
The NCQA Health Equity Measurement Framework, published in September 2022, details a multi-year effort supported by the California Health Care Foundation (CHCF) to “centralize equity in quality measurement through a set of domains that approach equity from a conceptually holistic perspective, with a parsimonious selection of associated quality measures that can be feasibly implemented into state accountability and incentive programs."
They engaged numerous stakeholders, including two state Medicaid organizations, four health plans and community-based organizations, and four stakeholder advisory groups, like the HEDIS Health Equity Expert Workgroup (EWG). Their measure selection process identified over 300 measures from 16 existing quality and health equity frameworks as well as broader health equity literature.
The workgroup's goal was not to present a menu of quality measures, rather a curated set that should be implemented completely, or “in totus," to ensure consistent representation of core equity concepts. For feasibility, the measure list was constrained to a final set of 21.
Six health equity-related domains with 21 measures
What's novel is that the NCQA group reviewed these available measures as a way to repurpose relevant and useful data with a few additions so that payers can more easily comply. For many of the new measures, the NCQA encourages payers to review what data they may already have that could fulfill the need.
Figure 1 defines the framework's six domains and the core measures related to overall well-being, which are illustrated in more detail in Figure 2. They include:
- Equitable social interventions
- Equitable access to care
- Equitable high-quality clinical care
- Equitable experiences of care
- Equitable structures of care
- Overall well-being
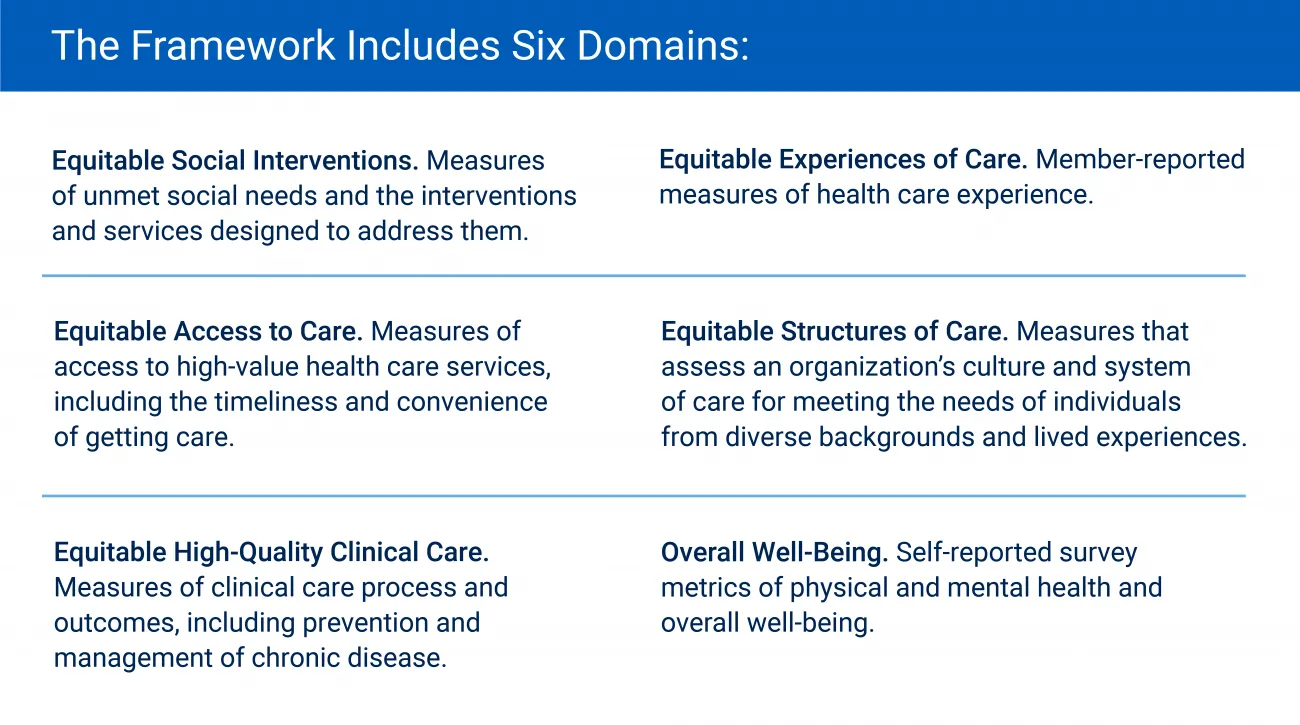
Figure 1: NCQA Health Equity Measurement Framework Domains
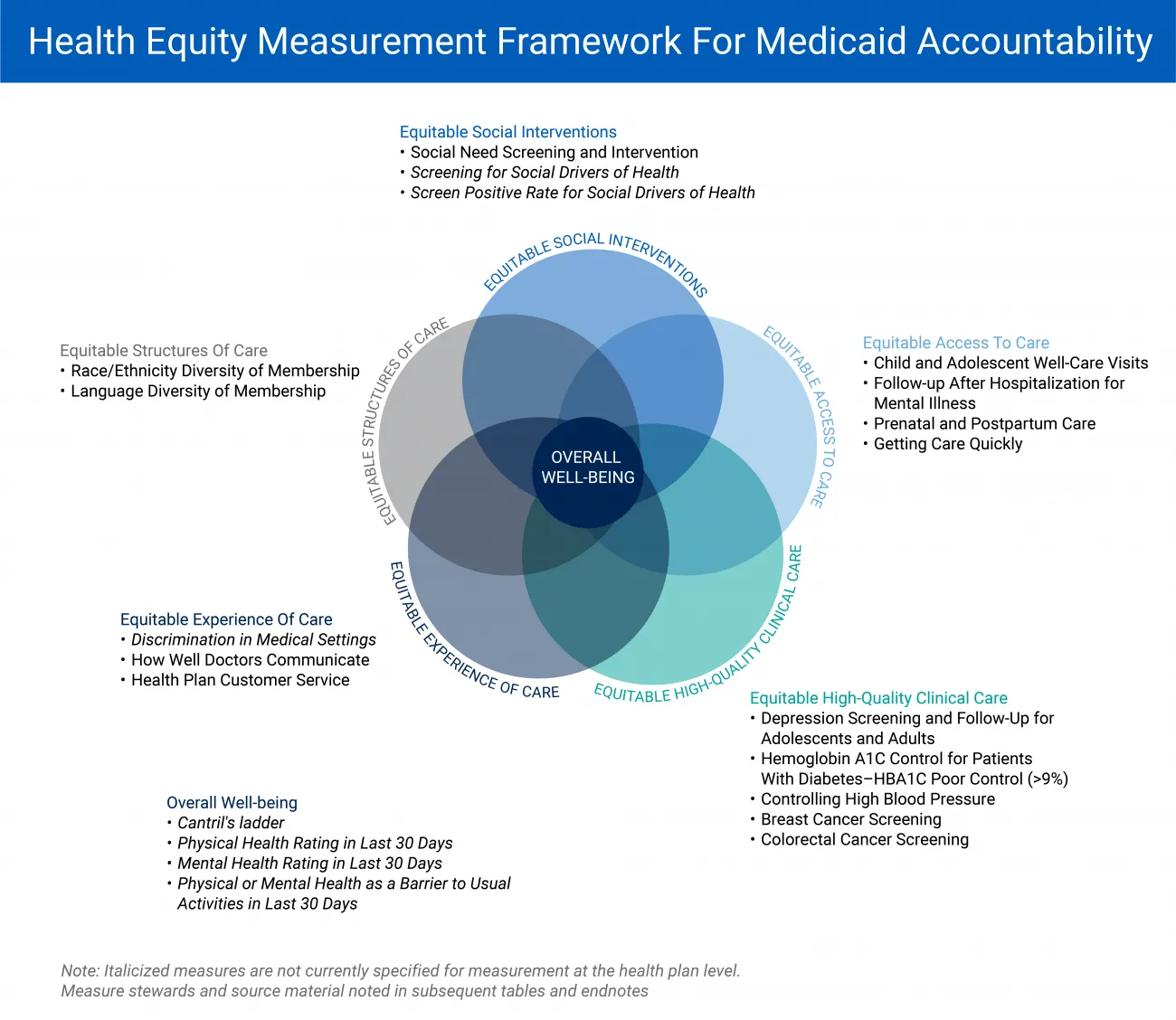
Figure 2: The framework includes six domains, as well as the area “Overall well-being." The figure outlines the 21 measures across the six domains.
The framework expands equity as a cross-cutting concept central to all domains of healthcare quality. This was achieved by adhering to eight guiding principles shown in Figure 3.
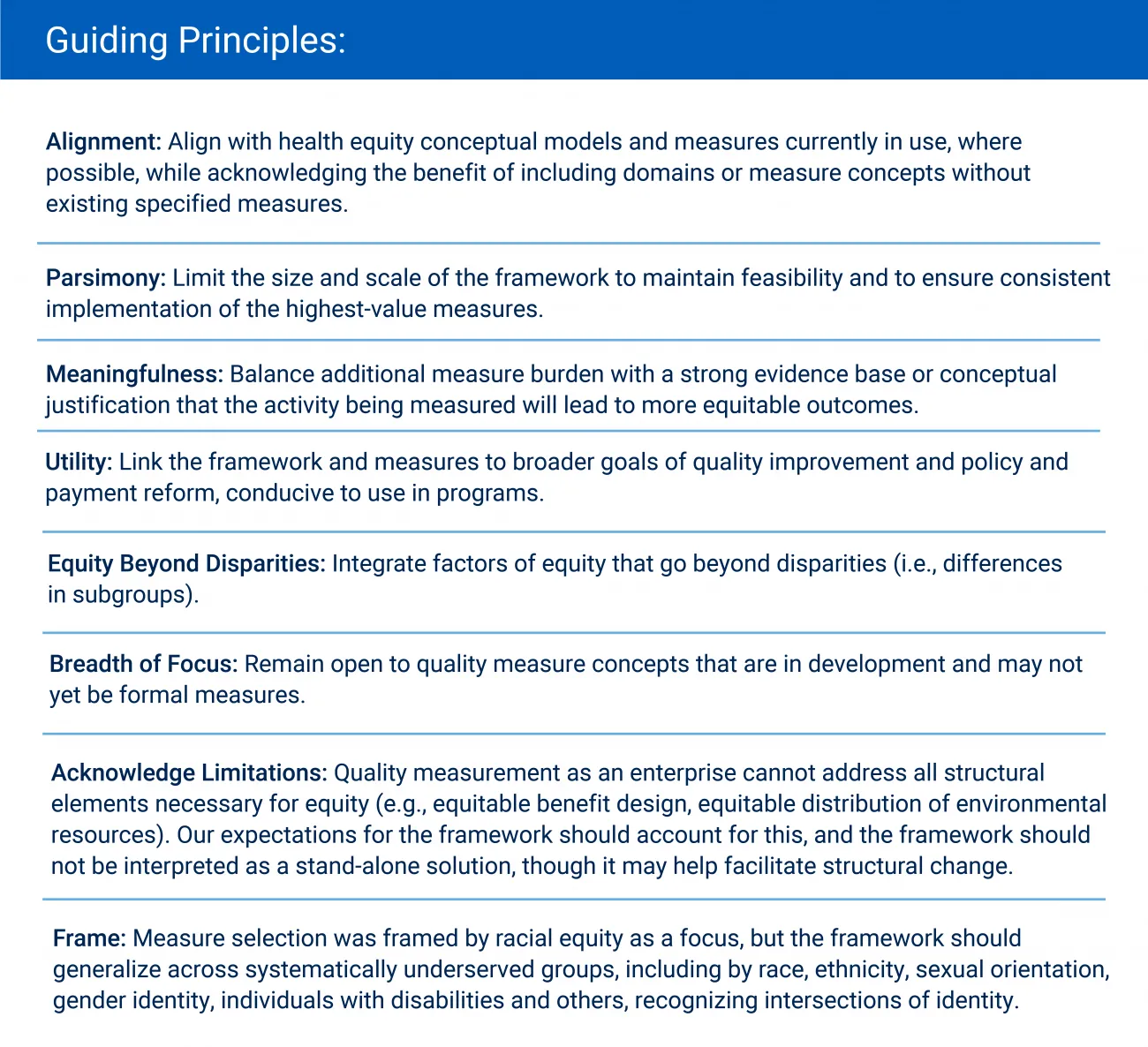
Figure 3: NCQA guiding principles for the development of the health equity measurement framework.
Health equity measures across the six domains
Figure 2 shows the framework as a flower shape, which connotes the NCQA's desire to avoid implications of hierarchy. They stress that “achieving equitable health care and outcomes require success across domains."
The following breakdown of the six domains, plus overall well-being, demonstrate NCQA's desire to leverage existing measures (like HEDIS®) and tools (like CAHPS survey), supplementing only with additional EMR, survey, or administrative data when necessary. Specific measure definitions can be found in the NCQA Health Equity Measurement Framework white paper.
Equitable social interventions
The NCQA suggests three measures in this domain:
- Social Need Screening and Intervention comes from HEDIS® and NCQA and can be acquired through an EMR.
- Screening for Social Drivers of Health comes from The Physicians Foundation and clinical source data.
- Screen Positive Rate for Social Drivers of Health also comes from The Physicians Foundation sourced from clinical data.
Equitable access to care
The NCQA suggests four measures in this domain. Three come from HEDIS NCQA's measures sourced from administrative data. The fourth is Getting Care Quickly that is sourced from CAHPS® survey data.
Aligned with top-line Medicaid priorities, the three NCQA measures center on child and adolescent well-care, mental illness hospitalization follow-up, and prenatal/postpartum care
Equitable high-quality clinical care
Sourced from administrative or EMR data, all five NCQA measures for this domain come from existing HEDIS scores. They focus on depression screenings and follow-up, diabetes control, high blood pressures control, and screenings for breast and colorectal cancer.
Equitable experiences of care
This domain's data covers three measures all sourced from survey data, including discrimination in medical settings and two CAHPS measures focused on how well doctors communicate and health plan customer service scores.
Equitable structures of care
Two NCQA HEDIS measures are suggested, which can be sourced from member-reported and enrollment data. They capture membership race and ethnicity diversity and language diversity.
Overall well-being
The last domain is at the center of the previous six. This domain suggests the “Cantril Ladder" (aka “Cantril's Ladder of Life Scale") —Dr. Hadley Cantril's "self-anchoring scale"— be used to assess whether a person is thriving, struggling, or suffering. The three others are derived from CDC measures:
- Physical health rating in the last 30 days
- Mental health rating in the last 30 days
- Physical or mental health as a barrier to usual activities in the last 30 days
Figure 4 provides a measure description of the core, overall well-being measure. They rely on the Behavioral Risk Factor Surveillance System (BRFSS), which is the world's largest continuously conducted health survey system. Launched in 1984, the system is updated through more than 400,000 adult interviews each year.
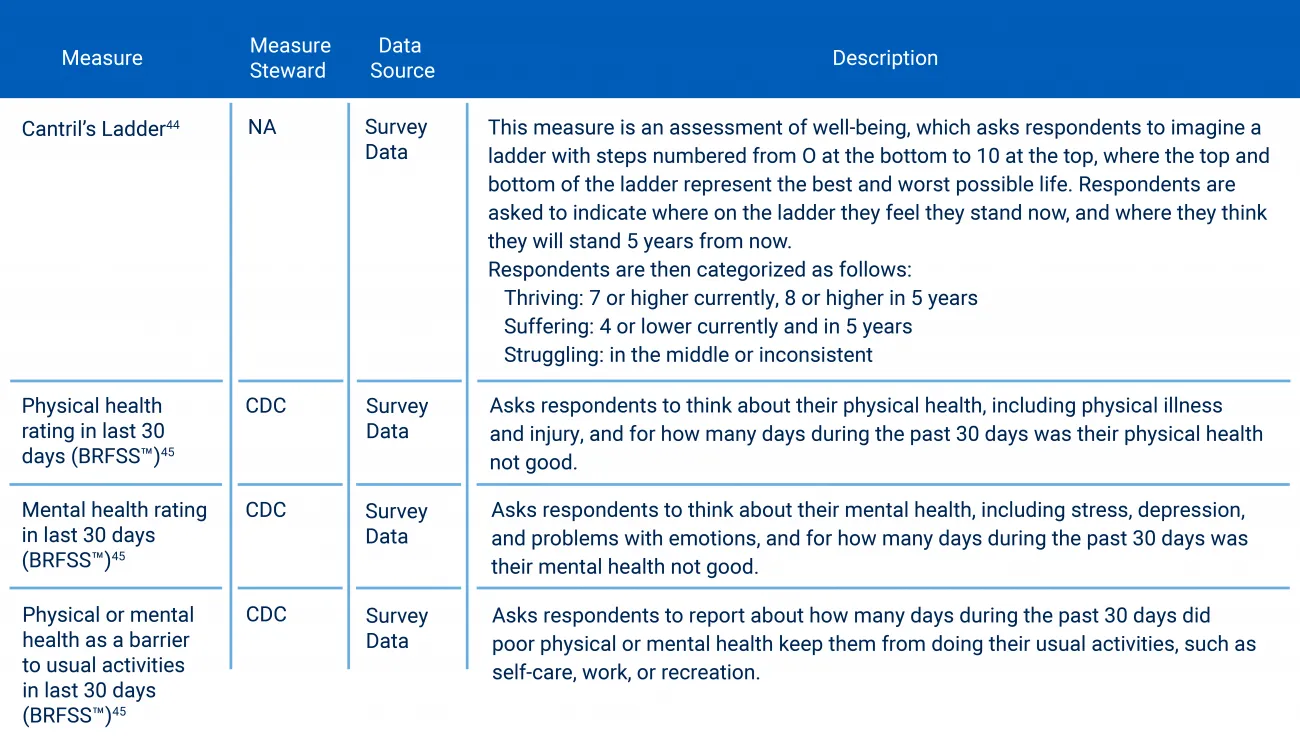
Figure 4: Overall well-being domain measures. Source: NCQA Health Equity Measurement Framework.
Health equity measurement is a critical part of improving Medicaid care quality
The 21 measures from the NCQA Health Equity Measurement Framework were selected based on six criteria: relevance, validity, reliability, feasibility, scientific soundness and relationship to outcomes. Stakeholders who were engaged throughout the development process reflect the breadth of the Medicaid ecosystem: state agencies, MCOs, patient advocates, community-based organizations, clinicians, and health equity researchers.
The framework outlined here is a critical part of a larger NCQA project that will evaluate and develop standard approaches to measuring health equity in Medicaid quality programs. Ultimately, this work provides the foundation for states to partner with healthcare organizations toward reducing disparities and improving accountability for equitable care.
Which states are adopting health equity measurement and requiring the same?
Part 2 in this two-article series will highlight how states are specifically incorporating health equity measurement into their programs via managed care contracts, state plan authority, section 1915 waivers, section 1115 demonstrations, and other initiatives.
Accelerate adoption of health equity measures toward improving reporting and performance.
RTI Health Advance supports states, payers, and communities in their pursuit of health equity performance measurement and quality improvement. Schedule an initial discussion with one of our health equity experts.
Subscribe Now
Stay up-to-date on our latest thinking. Subscribe to receive blog updates via email.
By submitting this form, I consent to use of my personal information in accordance with the Privacy Policy.